Why Do I Have Anxiety After a Concussion?
Concussions go far beyond just physical symptoms like headache, nausea, and dizziness. They even go beyond the cognitive aspects, such as brain fog and memory problems. Concussions often come with a variety of mood complaints like anxiety, depression, or worsening of pre-existing conditions like OCD or ADHD. If this is you, you’ll likely already know that the issue isn’t as easy as getting a prescription from a psychiatrist (sometimes that makes it worse).
If all this sounds familiar, we’re sorry you’re struggling, and you’re certainly not alone. Upwards of 65% of patients experience some form of mood disturbance after a concussion.
Concussions also tend to make pre-existing anxiety worse, leaving previously effective methods helpless in the wake of the new injury. It can feel hopeless, scary, and frustrating to not have a handle on anxiety following a concussion, and this article will help you understand why it’s happening and what to do about it. In this article, we’ll cover
-The experience of anxiety after a concussion
-Why anxiety happens after a concussion
-Common sources of post-concussion anxiety
-Treatment options
-Medical and non-medical options
If you’re reading this and you or someone you love is struggling with ongoing post-concussion anxiety symptoms, click here for a free consultation with one of our doctors. The Neural Connection specializes in stubborn post-concussion symptoms. Our doctors will carefully listen to your situation and make the appropriate recommendation, even if it’s not with us. Click here to schedule a consultation, and click here to see our 100+ 5-star reviews from people just like you.
The Experience of Anxiety After a Concussion
Anxiety is a mental state often described as excessively nervous, restless, or worrisome in the absence of any real threat to your safety. It is often accompanied by hyper-vigilance, where you may over-attend things in your environment because you don’t feel entirely safe. You may feel sweaty, tense, and sick when things get ramped up. Other ways patients have described it are:
-Not being able to wind down
-Racing thoughts that won’t stop
-Catastrophizing scenarios
-Being “wired but tired”
-Worrying that you’re worrying too much (the snowball effect)
-Lying awake at night due to intrusive thoughts
-Impending sense of doom
-Not being able to relax your muscles, especially around the neck
There are also specific scenarios that will be especially provoking following a concussion. Car rides, grocery stores, malls, or any place where there is a lot of sound and movement will potentially trigger a stress response and, consequently, an anxiety response. When concussion symptoms get touchy, the body creates the same stress hormones as when you’re anxious. These stress hormones circulate and team up with your emotional anxiety, creating a synergy that drives anxiety up even further.
Sometimes, without warning or any provoking event, the body will decide it’s going to ramp up the sympathetic nervous system and give you all the physical sensations of extreme anxiety, with little to no explanation or warning. When your heart rate increases and your breathing gets rapid and shallow for no reason, oftentimes, people will report having a panic attack. These are incredibly unpleasant attacks of stress that many report as feeling like “they’re going to die.”
Anxiety is a complex condition that has several branches to it, so understanding which parts are real anxiety and which parts are more of a fear response is helpful in long-term management. In the next section, we’ll explain what anxiety is and how to differentiate it from other similar reactions, like fear, anger, and post-conclusion flair-ups.
Causes of Anxiety After a Concussion
Anxiety after a concussion can come from a variety of different sources, some emotional and some physical. Concussions, commonly referred to as mild traumatic brain injuries (mTBI), often affect the brain’s ability to regulate something called the autonomic nervous system (ANS).
The autonomic nervous system balances the “fight or flight” branch and the “rest and digest” branch. This see-saw-like balance of activity helps counteract stress responses with things that calm your body and brain.
Around 35% of patients will experience prolonged ANS symptoms following a concussion. They may develop something called postural orthostatic tachycardia syndrome (POTS), experience panic attacks, have one pupil larger than the other, or get symptom flair-ups following exercise.
The point is that if a concussion disrupts the ANS, the body loses its ability to modulate stress responses. When this happens, the stress responses from anxiety can become more potent or more straightforward to provoke. Furthermore, the physical stress created by symptoms can either mimic anxiety or exacerbate anxiety that is happening during the flair-up.
This is the main reason why previously effective methods of managing anxiety are no longer effective once a concussion is introduced. More to come on that.

Photo Credit: Dr. Ryan Cedermark
How The Brain Interprets Threats
There is a substantial amount of hardware in the body designed to respond to danger. This circuitry is hardwired into most creatures on the planet to ensure they are hardwired to escape danger. Think of things like a puffer fish inflating to deter predators. The human system has a slightly different alarm system, and it has three components: fear, anxiety, and anger. Think of it as three different ways to trigger the same alarm system.
Think of these three alarms as the past, present, and future branches. The anger branch has more to do with past experiences and occasionally immediate situations. You may ruminate on someone who may have been at fault for an injury, an argument with a spouse/co-worker, or a current situation where you feel wronged by someone. The anger branch will physically prepare you for a confrontation, elevating levels of hormones responsible for actual “fight or flight” scenarios.
The fear branch is more concerned with immediate threats. Think home intruders or someone trying to hack your internet browser. When this branch is activated by something threatening, it’s designed to create a strong and immediate response to prepare the body for action. Rapid increases in adrenaline and cortisol cause shallow breathing, dilate pupils, and increase blood pressure. If you have existing autonomic issues from a concussion, this can initiate a symptom flair and an autonomic episode.
The anxiety branch is activated when worrying about the future. You may ruminate on uncertain scenarios in your life, if you’ll ever recover from your injury, or even worry about worrying. The physical response to this alarm is more subtle than the immediate response of the fear branch, but it can still worsen and create physical symptoms. This branch is especially active after a concussion, especially ones that produce chronic symptoms. As failed treatments begin to stack up, it’s easy to wonder if you’ll ever return to everyday life.
All of these can be active together, making it hard to tell where the anxiety is coming from. Now, let’s dive into why anxiety is so much worse following a concussion.
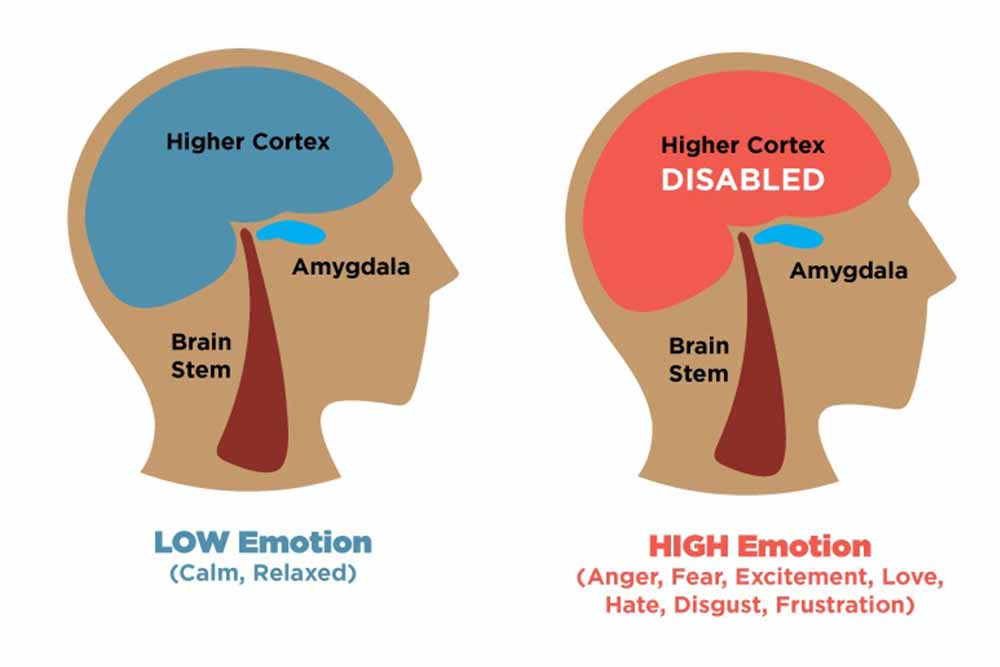
Photo Credit: Simply Psychology
Ways Concussions Promote Anxiety
Anxiety after a concussion can stem from several root causes. Some are more of what’s called a secondary cause, meaning it’s a symptom of the concussion. Other sources are directly resulting from the concussion and its overactivation of the ANS. We’ll take a look at a few sources below.
Dizziness and Sensory Mismatches
Dizziness is a common symptom after a concussion, affecting between 85-90% of patients within the first 3 weeks. When you look at dizziness, it’s essential to break it up into central and peripheral causes. Medical specialists efficiently treat peripheral dizziness like PTs or an EENT specialist. These are things like BPPV or Meniere’s disease.
Central vertigo involves a mismatch between the three systems that govern equilibrium: the eyes, the neck, and the vestibular system (think balance). When these systems don’t say the same thing, the body creates a strong stress response and a burst of dizziness. It’s similar to the sensation you get off a spinny ride, or if you’re at a stop light and the car next to you moves, you’re not sure you’re the one moving.
If you’re struggling with dizziness after a concussion, the physical response to these miscommunications can make existing anxiety worse or induce anxiety due to the hormonal response.
PTSD From the Accident
We see a lot of post-auto-accident cases, and it’s very common for people to get strong anxiety responses whenever they drive. These stored traumatic memories imbed themselves in the emotional processing centers in the brain. These centers, often called the “limbic system,” activate a stress response whenever they are thought of or when you’re back in a situation that led to an injury.
Furthermore, if you’re dealing with a complex collection of symptoms involving the eyes and vestibular system, driving itself can provoke symptoms. Many will report nausea and motion sickness following an injury, which we know causes a stress response that closely resembles anxiety.
Digestion Issues
It’s common for people to have digestion issues following a concussion. These issues can stem from a chronic state of stress, disruption of the gut lining, or damage to the brain region that communicates with the stomach. Whatever the cause, these issues can lead to leaky gut.
A leaky gut is a breakdown of the stomach lining that keeps the food you eat out of the bloodstream. This function is designed to fully digest the food and break down potential pathogens so they don’t circulate in the bloodstream. If someone has a leaky gut and continues eating the same foods, the stomach may fail to break down food completely, and you may circulate things you’re sensitive to.
Another aspect of stomach health that may enhance anxiety is the ability for the stomach to produce serotonin. When excessive stress causes the chemical environment to shift, the stomach has difficulty making enough serotonin to regulate your mood. Serotonin is often associated with depression, but it has ties to anxiety as well.

Photo Credit: Gastroenterology Consultants of Savanah
Ongoing Symptoms
The last way we see concussions affect anxiety is during a prolonged recovery with multiple unsuccessful treatment options. It takes a lot of physical, mental, and emotional energy to continually seek out treatments that might work. It’s especially alarming when several doctors tell you that everything is normal despite feeling symptomatic.
First, if any doctors tell you “there’s nothing more that can be done,” all that means is they’ve exhausted their specific toolbox, or they don’t know what else to do and don’t want to admit it. No one has all the answers, and providers aren’t always as humble as we’d like.
If you’re on the journey of a prolonged recovery and you continually run into anxiety issues, understand you’re not alone and this is a common, justified response. When you hear stats like “80% of concussions heal on their own”, it makes you feel like an outsider. The thoughts creep in, such as “am I stuck like this forever?”. Or, “I’m going to have to change how I live to adjust to this new normal.”
We’ll get into ways to manage these emotions later on. For now, let’s take a look at how the autonomic system can affect anxiety after a concussion.
Autonomic Dysfunction and Emotional Feedback Loops
The autonomic nervous system is divided into two main divisions. For simplicity, we’ll call them the stress response and the relaxation response. Normally, there is a see-saw-like balance between the 2, where the relaxation response can counterbalance the stress responses.
Issues with the ANS cause the see-saw to bottom out on the stress response side, causing a build-up of stress hormones and potentially fatigue of the relaxation response. When the stress response bottoms out, even without concussion symptoms, you’ll experience a rapid heart rate, shallow breathing, dilated pupils, and sweating. Many of these are similar to concussion symptoms, which makes it hard to tell the difference when they combine with other concussion symptoms.
This is an important point to understand. We frequently use this example in the clinic. Let’s say we offer you $1,000 if you can sit in a chair with your eyes closed and think about scary things until you create an autonomic response. This means you think anxious thoughts until your body responds to the emotional state. Most people say they would immediately take that bet because they always do it.
Then, we ask if they’d take the same bet if it were opposite, meaning they do something with their body until it affects their emotional state. Most are a little hesitant to take this bet as they’re unsure how they would do this. We then tell them this is the safest bet of them all because your concussion symptoms are doing it for you right now.
This is such an important piece of the puzzle because it shows you that anxiety is a continual cycle, where the emotional part feeds the physical, and the physical feeds the emotional. This is important because to fix the problem, you need strategies for both. We see too often a strategy that simply aims to reduce one big ball of anxiety, with no concern as to what individual parts are contributing.
In our experience, making progress with concussion symptoms and then addressing the emotional component has proven an effective way to attack post-concussion anxiety. The reduction in symptoms provides hope and relief that there might be a light at the end of the tunnel, which reduces anxiety by itself. Then, you’re not wrestling with the physical symptoms as much, which makes the emotional component easier to manage.
Panic Attacks and Physical Symptoms
It’s hard to explain panic attacks to someone who’s never had one. Before I had my first panic attack in 2023, I never understood them. The only frame of reference I had was from a friend who told me they feel like “you’re going to die or something really bad is about to happen.”
In 2023, I had way too much work stress happening at once, and it created intense acid reflux while I was sleeping. One night, it was so bad that the reflux went up into my throat, and I jolted awake with shooting pain in my left arm. I was faint, dizzy, and was 100% convinced I had just had a heart attack and I would die on the way to the hospital. Spoiler alert: I didn’t die and i got a hard lesson on what panic attacks are.
Panic attacks can happen both ways, meaning from physical causes or emotional responses like PTSD. In the case of concussions, they’re often a combination of both. Let’s look at how each component can contribute to panic attacks.
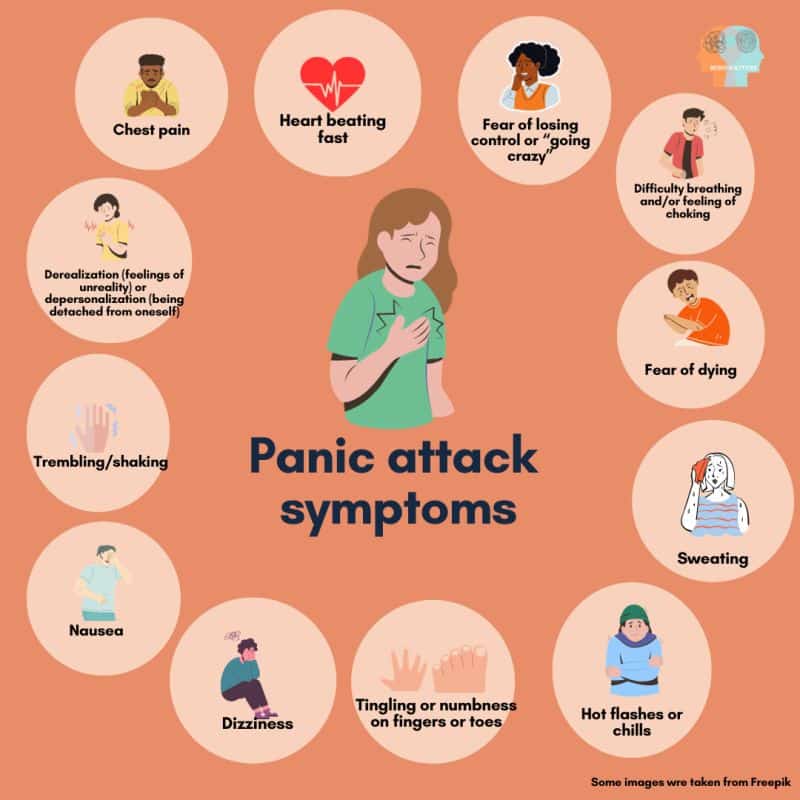
Photo Credit: Eleni Zenonos
Physical Symptoms
Prolonged concussion recoveries come with a tendency to become overwhelmed by certain situations. Grocery stores, car rides and shopping malls are perfect environments to overwhelm a touchy system. They’re loud and bright and have a lot of visual stimulation that can immediately create enormous amounts of stress and overwhelm.
Such a sudden dump of stress is perceived by your brain as dangerous and threatening, possibly leading to a panic attack.
Speaking from experience, when you feel your body acting as if it’s in danger, it’s nearly impossible not to feel some form of emotional fear as well. It’s especially alarming when you feel your body reacting to the stress and can’t figure out why or what’s causing it. When you react emotionally, you create an even bigger stress response and the snowball begins.
Trauma Responses
With enough exposure to these high stress environments, you can develop trauma responses to situations that have previously triggered a panic attack. We see this all the time in cars if the injury happened while you were driving. Your brain creates a strong emotional response tied to the situation that caused the injury. Every time you put yourself back in that situation, the brain triggers the trauma response, and you immediately feel a burst of fear and autonomic symptoms.
This can happen in the example above, too. If you get panicky every time you go shopping, you may develop these emotional responses before going into the store. This emotional response will bring the entire system closer to a panic attack before the physical symptoms have a chance to come on.
The overarching theme here is this: the physical and emotional components of anxiety after a concussion feed into each other. You need strategies for both to effectively manage them over time.
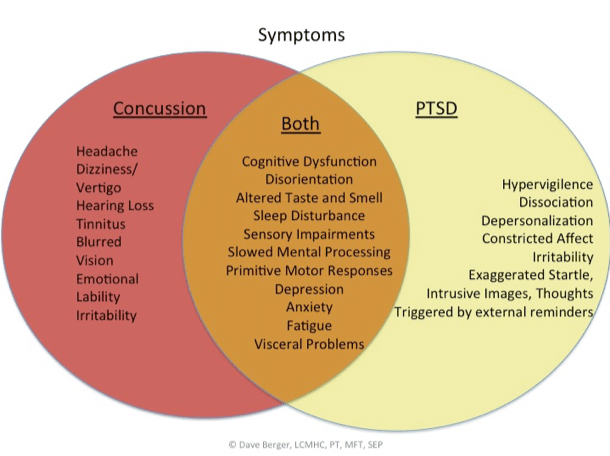
Photo Credit: Dave Berger
The Path Forward: Concussion Symptoms
If any of this content has resonated with you, there is a path forward. We’ve seen it work hundreds of times, and it all starts with getting your concussion symptoms and autonomic system under control. After this, managing emotional symptoms is a fair fight that you can win.
Below is an outline for how to best treat concussion symptoms based on our experience working with concussion patients with anxiety.
Concussion Rehabilitation: Autonomic System
The first priority in any concussion program is to ensure your autonomic system isn’t the root of the problem. There are a few easy ways to do this at home. The first involves something called the “Buffalo Concussion Treadmill Test.”
This test lets us see a snapshot of your autonomic health and reveals the most touchy symptoms. It begins on a treadmill or a stationary bike. After 5 minutes of light warmup activity (around 3-3.4 mph), increase the incline every minute until you feel symptoms. Measure your heart rate, and take note of what symptom/symptoms came on first. Click here for a tutorial.
This will tell you 3 things.
1: It will give you a prescription for exercise intensity. This means you take the heart rate that produced symptoms, take 80% of it (for example, symptoms came on at 140 bpm, and 80% of 140 is 112). Now, exercise at a heart rate of 112 every day until you re-assess in a week. Ideally, the heart rate that produces the symptoms will increase slowly, allowing you to push yourself harder each week. This will build durability, and cardio helps oxygenate brain tissue and create hormones that assist in rehab.
2: It will reveal which symptom is the easiest to provoke. These symptoms give you a good idea of where to start your search for relief.
3: If your symptoms persist well into the day, you can safely assume your autonomic system is at the root of the problem.
Symptom Assessment: How to Save Time
We use the analogy of a Rubix cube for concussion recovery. We live in a world of specialists, and each specialist works on their side of the Rubix cube. If you’ve ever done a Rubix cube, you know that working on one side often scrambles up the other. When you’re dealing with visual symptoms, dizziness, headaches, and anxiety, you’ll often end up with an eye doctor, a PT, a chiropractor, and a therapist all telling you different things to do.
Our clinic, The Neural Connection, gets around this problem by assessing a little of everything and using this information to cut right to the chase. By asessing the eyes, neck, vestibular system, emotional system, cognitive system, and autonomic system, we’re able to get a holstic, big picture view of everything contributing to your symptoms. We may not be able to treat every aspect, but we’ll be able to save you time, energy, and money by giving you a detailed view of all contributing factors. This allows you to make the most informed decision about who to seek care.
Let’s look at one of our patients as an example. She came in to see us after trying vestibular therapy, vision therapy, chiropractic, and medication. Vestibular therapy and chiropractic made her more dizzy, vision therapy helped a little but the prism glasses gave her more headaches, and the medication gave her other unwanted symptoms.
We worked around this by addressing things in the right order. She couldn’t do vestibular rehab because moving her neck caused symptoms, so we treated her neck before beginning vestibular therapy. Once we could treat the vestibular issues with a pain-free neck, the visual exercises worked because the eyes no longer competed with the vestibular system. Once we treated her visual problems, her autonomic symptoms nearly went away, and completely resolved once we referred her out to a therapist to treat the remaining anxiety issues.
If you’re reading this and you or someone you love is struggling with ongoing anxiety after a concussion, click here for a free consultation with one of our doctors. The Neural Connection specializes in stubborn post-concussion symptoms. Our doctors will carefully listen to your situation and make the appropriate recommendation, even if it’s not with us. Click here to schedule a consultation, and click here to see our 100+ 5-star reviews from people just like you.

Anxiety Medication
People will often go on one of two types of anxiety medication: SSRIs and beta blockers. Consider the following information when deciding whether or not to go on medication for anxiety.
SSRI Research is Mixed at Best
The statistics show mixed results with SSRI medication for anxiety. Around a third see relief, roughly a third see little relief, and another third see no relief. Most of our patients describe a process that seems like guesswork at best. They often try a dose, and if it doesn’t work, up the dose or try a new medication until they either succeed, give up, or the side effects pile up, and the patient self-selects off the medication. Always remember you’re the boss in any medical setting, regardless of how it feels. If you’re not responding to the medication or it gives you new side effects you don’t want, advocate for yourself and don’t let them bulldoze you. That goes for any provider, even us. Your health is the most important thing, and healthcare workers work for YOU, not the other way around.
Medication Side Effects
There are a few important things to consider when going on medication. The most important is to look for side effects that overlap with your symptoms. We had a migraine patient come in with intense dizziness during attacks. It was so intense she couldn’t drive or walk without support. We tried rehab, but got nowhere until we looked into her anxiety medications and found 2 of them had dizziness as a side effect. We spoke with her physician to transition her off, and her dizziness resolved almost immediately.
Another aspect to look out for is nutrient depletion. Many medications cause nutrient depletion, which can mimic primary symptoms of medication side effects. Make sure you double-check what nutrients are susceptible to depletion whenever you start a new medication.
Beta-blockers are not a long term fix
Beta-blockers are not meant to be taken over the long term. They’re used as a fallback when symptoms flair and can often interfere with the rehab process because they tend to subdue the entire nervous system. However, if you’re in a pinch and need relief immediately, they can be effective in the short term. Make sure you’re aware of this before beginning a treatment regime.
Helpful Tips to Manage Anxiety After a Concussion
While these options are no substitute for a comprehensive, integrated plan, we’ve found many of these tools helpful for managing anxiety after a concussion.
Vagal Nerve Stimulation
The vagus nerve is responsible for counteracting stress in the body. Connections run down your heart, lungs, and intestinal tract to ensure prolonged stress doesn’t build up. We use a device called Truvada to naturally stimulate the vagus nerve and relieve some of the unwanted effects of anxiety.
Neurofeedback
Neurofeedback is a meditation on steroids. It measures your brain activity, identifies the patterns that correlate with anxiety, and trains the brain on how to produce better activity. It’s safe and noninvasive, and anxious people typically respond well.
Meditation and Deep Breathing
The autonomic system is largely outside of conscious control. One of the only ways you can directly influence it is through the speed and depth of your breathing. Activities like mindfulness meditation and deep breathing have been shown to reduce anxiety and help cope with uncomfortable emotions.
Low Glycemic Diet
When blood sugars fall too low, your body produces a small stress response so your body can pull sugar out of storage. As a best practice, choosing to follow a low glycemic diet takes this burden off your body and allows for better management of the autonomic system.
EMDR
EMDR is a therapy designed to reduce the emotional charge of stressful stored memories. If you’re dealing with any sort of PSTD or having trouble shaking the emotional after-effects of a concussion, EMDR can be a great way to turn down the volume of those intrusive thoughts.
A word of caution: if you have ocular symptoms and get overwhelmed by a lot of visual activity, rehab those symptoms before beginning EMDR.
Counseling and Support Groups
Concussions are often referred to as “invisible Injuries.” To the outside world, you appear normal, but inside, you know things are anything but. Counseling and support groups are a great way to feel less isolated. Hearing stories similar to yours and talking with someone who can validate your concerns and guide you to helpful practices can make all the difference in the world.
Conclusion
Anxiety after a concussion can be a hard, isolating journey full of ups and downs. We hope this article helps shed light on some of the sources of anxiety and helps you understand how concussions and anxiety go hand in hand. Always remember: you’re not alone, and this too shall pass.
If you have questions about concussion recovery, click here to schedule a complimentary consultation with one of our doctors. We’ve treated hundreds of complex neurologic cases and can help piece together the missing pieces in your recovery.
*Note: The information provided in this article is for educational purposes only and does not constitute a doctor-patient relationship. Patients should consult their medical provider or primary care physician before trying any remedies or therapies at home.
