A traumatic brain injury (TBI) can flip your sleep quality upside down. Many TBI survivors struggle with insomnia – difficulty falling or staying asleep. Others battle with relentless drowsiness, needing far more sleep than before. These sleep disturbances are a common yet often overlooked consequence of TBI. Studies estimate that anywhere from 30% to 70% of people with TBI experience some form of sleep problems as a result of their injuries.
These changes in sleep can happen immediately after the injury or even months later. If you’ve sustained one or more TBIs (including concussions) and find yourself sleepless at night or exhausted all day, you are not alone.
Sleep issues after a brain injury aren’t just an annoyance; they can significantly impact your recovery and quality of life. Lack of restful sleep makes it harder for the brain to heal, affecting memory, mood, and energy levels. It can also worsen other post-TBI symptoms like headaches, depression, anxiety, and irritability.
These issues create a vicious cycle: your brain injury disrupts your sleep. This poor sleep, in turn, slows your brain’s healing and aggravates your symptoms. The good news is that treating these issues with adequate education, understanding, and personalized treatment options is possible.
You can improve your rest and support your brain’s recovery by addressing sleep issues. Ideally, this would occur in a personalized and holistic manner, along with other structural, neurological, and metabolic factors.
In this post, we’ll cover:
- Types of Sleep Problems After a TBI – the common sleep disturbances TBI patients experience, like insomnia, hypersomnia, and more.
- Causes of Post-TBI Sleep Issues – why brain injuries disrupt sleep, including direct brain changes, hormonal imbalances, and other factors.
- Treatment Options for Sleep Problems – from sleep hygiene and lifestyle changes to therapies and medications that can help.
- Why a Holistic Approach Is Important – why treating sleep in isolation may not be enough, and why there is a need to address underlying issues.
- The Neural Connection’s Integrative Approach to TBI Recovery – how our patient-centered team helps TBI patients overcome sleep problems through a comprehensive program that addresses the whole person.
Understanding the connection between TBI and sleep is the first step toward finding answers. You also deserve personalized and practical solutions that promote healing and long-term well-being.
If you or a loved one is suffering from post-TBI sleep difficulties, know that help is available. The Neural Connection’s integrative team is here to empower you with education and therapies that treat the root causes of your sleep problems.
You don’t have to settle for sleepless nights or groggy days – recovery is possible.
If you feel ready to seek professional help, we would love to chat. Contact our providers at The Neural Connection for a free consultation to discuss your situation.
Types of Sleep Problems After a TBI
After a traumatic brain injury, “sleep problems” can mean many different things. Every individual’s experience is a bit different. And at the end of the day, finding ways to maximize sleep is essential for healing and recovery.
Here are some of the most common types of sleep disturbances TBI patients encounter:
Insomnia
Insomnia is described as trouble falling asleep, staying asleep, or waking up too early. Sadly, it’s the most common sleep complaint after TBI. About half of TBI patients experience insomnia at some point. You might lie awake for hours or wake frequently at night and struggle to get back to sleep. These sleep issues usually leave you feeling unrefreshed and tired during the day. Post-TBI insomnia often worsens cognitive problems (like poor concentration and memory) and mood issues. The good news is it can improve over time and with proper treatment.
Excessive Daytime Sleepiness (Hypersomnia)
The opposite of insomnia, some TBI survivors feel sleepy all the time. This presentation can manifest as sleeping much longer than usual at night or needing multiple naps during the day. Post-traumatic hypersomnia (including conditions like post-traumatic narcolepsy) affects roughly 25–30% of TBI patients.
People with this issue may sleep 10–12+ hours and still feel groggy or find themselves falling asleep suddenly during the day. Hypersomnia also correlates with troubles in cognitive focus, memory, and persistent fatigue.
Circadian Rhythm Disturbances
TBIs can disrupt your body’s internal clock. Some patients develop irregular sleep-wake cycles or a shifted schedule following their injury. For example, you might be wide awake at night and sleepy during the day, a reversal of standard wake-sleep patterns. In other cases, sleep may fragment into multiple short bouts throughout the day.
These disrupted patterns (sometimes called circadian rhythm disorders) make it challenging to maintain a routine. You may experience fragmented sleep and bouts of extreme drowsiness at the wrong times. Research shows that about one-third of people with brain injuries show shifts in their sleep-wake cycle weeks to months after the injury. This pattern can be very frustrating and often interferes with work, school, and daily life.
Parasomnias (Abnormal Sleep Behaviors)
A significant number of TBI patients (estimated ~25%) experience unusual behaviors during sleep. Parasomnias can include symptoms of sleepwalking, talking in your sleep, intense nightmares, teeth grinding, or even acting out your dreams (called REM behavior disorder).
Parasomnias can be upsetting or potentially dangerous (for instance, if you sleepwalk and injure yourself). When present, they often indicate an alteration in the brain’s sleep architecture. Nightmares and vivid dreams, in particular, are commonly reported after TBIs and may be linked to PTSD or the brain injury itself.
Sleep-Related Breathing Problems After A TBI
Sleep-disordered breathing, especially sleep apnea, is also more common after TBI. Around 20% of TBI patients develop sleep apnea, a medical condition where you repeatedly stop breathing for brief moments during sleep. These symptoms often lead to loud snoring, gasping, or choking while awake and fragmented, poor-quality sleep.
Sleep apnea after a brain injury can stem from changes in the brain’s control of breathing or injury-related factors like weight gain and reduced muscle tone in the airway. It often causes severe daytime fatigue, morning headaches, and concentration issues due to the brain getting less oxygen at night.
These various sleep disturbances can occur singly or in combination. For example, a person might have insomnia some nights and hypersomnia other days, or sleep apnea that leads to insomnia. It’s also common for sleep issues to evolve over time. Patients might have acute insomnia right after the injury and then develop a circadian rhythm issue later on.
Proper diagnosis is key because different sleep problems often require different treatments. If you’re dealing with any of these sleep problems after a TBI, discussing them with a healthcare provider is essential. Sleep problems are not minor annoyances; Sleep is an integral part of your recovery puzzle.
If you’re unsure what kind of sleep issue you have, reach out! The team at The Neural Connection can help evaluate your symptoms and/or help you find the right provider for treatment.
Don’t hesitate to reach out for a free consultation – we can help you identify the problem and chart a path forward, whether in our office or elsewhere!
What Causes Sleep Problems After a TBI?
Why do traumatic brain injuries wreak such havoc on sleep? The causes can be complex and multifaceted. TBIs often affect the brain in many ways. With that said, sleep is a delicate process that depends on a fully functional brain and body.
Here are some of the most common reasons TBI survivors experience sleep problems:
Direct Injury to Brain Regions that Control Sleep
Certain parts of the brain regulate our sleep-wake cycle. When damage occurs to the brain, like in a TBI, these networks can become disrupted. For instance, the hypothalamus (specifically an area called the suprachiasmatic nucleus) is like your internal clock, signaling your brain and body when it’s time to be awake or asleep.
The brain stem and the Reticular Activating System (RAS) network are crucial for maintaining consciousness and sleep transitions. A TBI – whether from a direct blow or the whiplash motion of the head – can damage these critical structures. If the neural circuits that control sleep become dysfunctional due to injury or trauma, the result can be insomnia, excessive sleepiness, or an erratic sleep pattern.
For example, direct damage to the retino-hypothalamic tract (the pathway linking your eyes to your brain’s clock) can interrupt your circadian rhythms and alter your sleep cycles.
How Light Plays A Role in Sleep Regulation
Typically, light signals from the eyes help the brain synchronize your sleep-wake cycle to day and night. If that connection is injured, your brain might not correctly register day vs. night. This can lead to issues like fragmented sleep or daytime sleepiness. This is one of the most common sleep problems after a TBI.
Similarly, diffuse axonal injury (the stretching/shearing of brain cells common in concussions) can disturb communication within sleep-regulating networks and affect all of these central areas of the brain.
In addition, TBIs often involve both the brain and the neck. Whiplash and neck injuries can cause lesions or damage to nerves and blood vessels, indirectly affecting sleep. Research has found that head-neck trauma can lead to conditions like hypersomnia and even contribute to sleep apnea.
For instance, injury to the upper cervical spine might impact brainstem function or breathing reflexes during sleep. The structural damage from an injury – whether in the brain’s sleep centers or related pathways – is one fundamental cause of post-TBI sleep disturbances.
Neurovascular Coupling Disruption
The brain relies on a process called neurovascular coupling (NVC) to function optimally. NVC is the mechanism by which active brain regions get more blood flow (and thus oxygen and nutrients) when needed.
*Fun Fact: This is the way that MRI technology works!
NVC acts like the brain’s fuel delivery system, making sure each part of the brain has the energy to do its job. Unfortunately, after a TBI, this process often gets disrupted.
When this process no longer functions, blood flow may no longer increase appropriately in response to neural activity, blocking oxygen flow and nutrient availability. When NVC affects the areas of the brain that manage sleep, your brain might struggle to maintain regular sleep cycles.
Think of it this way: If the circuits that help you fall asleep or stay asleep aren’t getting enough blood flow at the correct times, they can’t work correctly. The result can be insomnia (because the brain can’t shift into the “sleep” mode effectively) or constant sleepiness (if the brain can’t sustain alertness).
NVC problems are invisible injuries you can’t typically see on a standard MRI. They are metabolic and functional neurological issues that occur after concussions and TBIs.
That said, this could be one of the reasons why traditional scans might look “normal” even if you’re still having serious symptoms.
At The Neural Connection, we pay attention to these subtle neurological dysfunctions. By improving neurovascular coupling through targeted therapies (like aerobic exercise and neurorehabilitation), we aim to restore healthy function in those sleep-related brain areas.
It’s part of our personalized approach to treating complex neurological injuries.

Autonomic Nervous System (ANS) Imbalance
Your autonomic nervous system controls the background automatic functions of your body. Think of things like heart rate, blood pressure, breathing, and digestion. It has two branches: the Sympathetic Nervous System (SNS), which triggers “fight or flight” responses (alertness, adrenaline, etc.), and the Parasympathetic Nervous System (PNS), which promotes “rest and digest” (calm, relaxation, sleep).
Under normal conditions, these two systems balance each other. In healthy sleep, sympathetic activity gradually decreases, and parasympathetic activity increases. This is especially important during deep sleep, to slow your heart rate and relax your body.
Sadly, after a TBI, this delicate balance can be thrown off. Even a mild TBI or concussion can cause a state of dysautonomia, where the sympathetic system remains overactive and dominant over the parasympathetic system. In other words, your body might get stuck in a slight “fight or flight” mode.
Being in this state makes it very hard to switch to the relaxed “rest and digest” state needed for proper sleep. It also becomes a big sleep problem after a TBI.
Hyperarousal is a common issue post-TBI, where patients often describe feeling “amped up” or unable to shut off their brain at night. This heightened arousal is heavily correlated to insomnia and fragmented sleep patterns.
Here’s what typically happens as you start to fall asleep:
As your head hits the pillow and you drift off to sleep, your SNS (stress response) should dial down, and your PNS (calming response) will take over.
After a brain injury, the SNS may not shut off properly, causing you to remain too alert and stimulated. This elevated state can cause trouble falling asleep, changes with light or restless sleep patterns, and even cause physical symptoms like a fast heart rate at night.
Some TBI patients may also experience surges of SNS activity during REM sleep (when dreaming occurs), which can lead to nightmares or sudden awakenings with panic. Over-activation of the sympathetic system also correlates with sleep apnea and other sleep disturbances.
Therapies and exercises that help regulate the autonomic nervous system – such as biofeedback, breathing exercises, and specific neuro-rehabilitation techniques – can be beneficial.
Part of our approach at The Neural Connection is teaching your body how to wind down so that when bedtime comes, your nervous system can allow you to sleep deeply.
Hormonal and Neurochemical Imbalances
TBIs can disrupt the delicate balance of hormones and neurotransmitters that govern sleep. The injury might damage the pituitary gland or hypothalamus (key hormone controllers) or otherwise alter chemical signaling in the brain.
Research shows that TBI patients often have deficiencies in critical sleep-related neurochemicals like hypocretin (orexin), histamine, and Melatonin.
Here’s a breakdown of why these are so critical for sleep:
Hypocretin (Orexin) and Histamine Dysfunction Causing Sleep Problems After A TBI
Hypocretin (Orexin) and Histamine are neurotransmitters that help keep you awake and alert. In the literature, they are sometimes called wake-promoting chemicals.
After a TBI, hypocretin and histamine levels in the brain can drop significantly. Low hypocretin is famously linked to narcolepsy, and generally, if these chemicals are scarce, a person may experience excessive daytime sleepiness or an inability to stay alert (hence the hypersomnia some experience).
One study found that 95% of acute TBI patients had abnormally low hypocretin levels in their cerebrospinal fluid.
Reduced histamine activity (due to loss of histamine-producing neurons) has also been observed in severe TBI cases, with these changes pushing the brain toward a more sleepy state by day.
Melatonin and Sleep Dysfunction
Melatonin is a hormone that regulates the sleep-wake cycle, usually rising in the evening to help induce sleepiness. TBIs can cause decreased production or dysregulated release of Melatonin.
For example, patients with TBI have been shown to produce significantly less Melatonin at night than healthy individuals.
Without enough Melatonin or with altered release times, you might experience trouble falling asleep or experience lighter, less restorative sleep. Low Melatonin is associated with reduced REM sleep and poor sleep quality in TBI patients.
As you can see, the production and release of these hormones are essential to proper brain health. These hormonal imbalances can make it biologically hard to get restful sleep, even if your sleep environment and habits are perfect.
When Doing Everything Still Yields No Change…
You could be doing everything “right” and still struggle because your brain isn’t producing the appropriate signals for sleep. Identifying and addressing these issues is essential – whether through medical evaluation of endocrine function or using supplements or medications to help replace or boost these substances (for instance, taking Melatonin in the evening to help with sleep).
At The Neural Connection, part of our metabolic focus is checking for such imbalances and addressing them so your body’s chemistry can support healthy sleep. As you can see, healthy sleep is essential for recovery from a traumatic brain injury.
Other Sleep Problems After TBI and Co-Morbidities
Sleep problems after TBI often rarely occur in isolation. They frequently accompany other symptoms and conditions that feed and impact one another.
Chronic Pain Causing Sleep Problems After a TBI
For example, if you’re dealing with chronic pain (headaches, neck pain, etc.) due to your injury, that pain can keep you awake at night, altering your sleep in the process. Conversely, lack of sleep can lower your pain threshold and make pain feel even worse – a vicious positive feedback loop.
Mood Disorders and Mental Health
Similarly, mood disorders are common after TBI’s, as many patients can experience depression or anxiety. These conditions often cause disturbed sleep patterns. Racing anxious thoughts may cause insomnia at night, and depression may lead to insomnia, excessive sleeping, or a mixture of both.
Studies indicate that generalized anxiety disorder within the first few months of a TBI strongly correlates with the later development of chronic insomnia.
Fatigue and Exhaustion
Fatigue is another symptom that might seem simply like a consequence of poor sleep, but it can also cause sleep issues in a counterintuitive way. When you’re extremely fatigued, you might take long naps during the day or be unable to stick to a routine, disrupting your nighttime sleep schedule.
In these situations, TBI patients will often try to cope by increasing caffeine or other stimulants to fight fatigue, which can boomerang and cause insomnia or jittery sleep.
Cognitive Delays and Sleep Problems After A TBI
Cognitive symptoms like brain fog or dizziness can also add to the problem – for instance, being dizzy or nauseated can make lying in bed uncomfortable, or cognitive rest needs might conflict with building a daytime routine.
Additionally, post-traumatic stress (if the injury was tied to a traumatic event) can cause nightmares, night sweats, and heightened alertness at night. This can often worsen sleep problems after TBI.
All of these factors create a feedback loop: TBI causes symptoms like pain and anxiety, which make sleep harder; then, poor sleep exacerbates those symptoms. This is why treating sleep problems alone isn’t enough – one must also address the underlying symptoms and overall health. A genuinely effective recovery plan looks at the whole picture and creates personalized solutions.
These previously listed reasons are why, at The Neural Connection, we emphasize treating sleep disturbances and the co-occurring issues (pain, mood, cognitive deficits, etc.) to break out of this cycle and make real progress with our patients.
Medication Side Effects Causing Sleep Problems After a TBI
It’s very common for TBI patients to be on one or more medications, especially in the early stages after the injury. Unfortunately, many medications can impact sleep – sometimes in ways that seem ironic.
For example, your medical doctor may prescribe stimulant medications to help with daytime fatigue or focus. While stimulants can be helpful at times, they may also cause insomnia if taken too late in the day or if the dose is too high.
On the flip side, certain sedating medications might make you too sleepy or groggy during the day and into the evening, upsetting the standard sleep architecture.
Here are the most common medications that can negatively impact sleep and cause sleep problems after a TBI:
Antidepressants
Many people with TBIs take antidepressant medications to manage their mood or pain levels. Certain types (especially SSRIs and SNRIs) can cause insomnia or very vivid dreams in select groups of individuals.
Other antidepressants might have a sedating effect and cause daytime drowsiness. These effects often depend on the specific drug and the timing of the dose.
For instance, taking an antidepressant with activating effects (like fluoxetine) in the evening could keep you up at night, altering your sleep and negatively impacting your mood the following day.
Stimulants
Prescriptions for drugs like Methylphenidate (Ritalin) or Modafinil are often used to treat post-TBI attention problems or excessive daytime sleepiness. If not carefully managed, these can interfere with night sleep – particularly if taken too late in the day.
You should ideally take these medications in the morning or early afternoon to allow their effects to wear off by bedtime.
*Clinical Note: It’s always best to follow the instructions and guidance from your prescribing provider, especially before you try to modify your medication schedule.
Pain Relievers (Over-the-counter Medications & Opioids)
Over-the-counter (OTC) pain meds sometimes contain caffeine (Excedrin, for example, has caffeine along with analgesics). The caffeine contained in these medications could hinder your sleep if you’re unknowingly taking them in the afternoon or evening to manage pain or headaches.
Prescription pain meds (like opioids) can paradoxically disrupt sleep patterns as well. While they sedate you initially, they can have delayed effects that reduce restorative REM sleep and lead to fragmented sleep throughout the night (not to mention potential dependency issues).
Anti-Anxiety and/or Sleep Medications
Paradoxically, some medications used to treat sleep or anxiety, like benzodiazepines, if used long-term, can alter sleep stages and may lead to lighter sleep or tolerance (requiring higher doses). They can also cause next-day grogginess, impacting your daytime function and nighttime behavior.
As we’ve discussed, the key point is that medication side effects can create new sleep problems or worsen existing ones. Sometimes, adjusting the timing (e.g., taking a drug in the morning instead of at night), switching to a different medication, or tapering off a drug that isn’t essential can dramatically improve sleep quality.
*Clinical Note: We will never suggest stopping or changing medications on your own, but it may be worth reviewing your meds with your prescribing doctor if you have persistent post-TBI sleep issues.
At The Neural Connection, our team takes into account all the medications and supplements you’re on. We often collaborate with prescribing doctors or provide guidance on integrative alternatives to ensure that what you’re taking is helping your recovery, not hurting it.
How Are Sleep Problems Treated After TBI?
There is no one-size-fits-all treatment for post-TBI sleep disturbances. What helps you depends on the type of sleep problem, its severity, and its underlying causes. Typically, doctors and therapists will start with conservative, non-invasive approaches and only move to medications or more intensive treatments, if needed, based on your response.
Managing and treating sleep issues often becomes a stepwise process: Try one thing, and if it’s not enough, try the next until we see a positive change. Over time, the goal is to find a solution (or combination of solutions) that helps you get quality sleep regularly.
We’re going to explore the range of treatment strategies, from basic lifestyle adjustments to specialized therapies.
Sleep Hygiene and Lifestyle Changes
Improving your sleep hygiene should be the first recommended step in finding treatment. “Sleep hygiene” refers to the healthy habits and environmental adjustments that set the stage for consistent and restorative sleep.
After a TBI, it’s crucial to be disciplined about these habits because your brain may not regulate sleep as effortlessly as before. Small changes in your daily routine can significantly improve your sleep quality and quantity over time.
Here are some evidence-based tips to implement immediately:
Daytime Tips
Keep a Consistent Wake-Up Time
Get up at the same time every morning, even on weekends. A fixed wake-up time helps reset your circadian rhythm and reinforces a stable sleep-wake cycle for consistent and restorative sleep.
Stay Active and Engaged
If your current condition allows, engaging in meaningful daily activities can benefit your physical, mental, and emotional health. These activities include light exercise, cognitive tasks, social interactions, or engaging in hobbies.
Staying active (physically and mentally) can reduce daytime naps and build up your sleep drive for the night. Exercise, in particular, has numerous benefits for sleep – but we suggest avoiding intense workouts within a couple of hours of bedtime, as they might rev up your nervous system.
Limit Screen Time and Blue Light Exposure
Try to cut down on long periods of screen use, especially later in the day. The vibrant blue light emitted from phones, tablets, and computers can trick your brain into thinking it’s daytime, suppressing melatonin release and affecting sleep. If you must use devices in the evening, consider using blue light-blocking glasses or software that filters blue light.
Get Some Sunlight (or Bright Light) Each Morning
Exposure to natural light in the morning can help normalize your body clock. Open the curtains, sit by a window, or walk outside for a short walk when you wake up. In places with limited sun, a light therapy box in the early morning can also simulate this process (more on light therapy shortly). This daytime light exposure can also help improve mood and reduce fatigue.
Nap Smart, If Needed
It’s okay to nap, especially if you’re dealing with fatigue from your brain injury– but keep naps short and early. A 20-30-minute nap can be helpful in the early afternoon, as it can refresh you without cutting into your night’s sleep. Be careful, as long or late naps (e.g., 2-hour naps or napping in the evening) can sabotage your ability to fall asleep at night. If napping worsens your insomnia, you might need to avoid naps entirely for a while.
Nighttime Tips
Maintain a Consistent Bedtime
Just as with wake time, it’s best to try and go to bed at roughly the same time every night. This timing trains your brain when to expect sleep. Over time, a consistent schedule can make it easier to fall asleep naturally.
Have a Calming Pre-Sleep Routine
Spend the final 30-60 minutes before bed doing relaxing activities without screen time. This could include reading a light book, listening to soothing music or nature sounds, gentle stretching, deep breathing exercises, or journaling.
Many people with TBI find mindfulness meditation helpful in calming an overactive mind at night. A warm shower or bath in the evening can also help your body temperature dip afterward, promoting sleepiness and better sleep.
Create a Sleep-Friendly Environment
It’s essential to optimize your bedroom for sleep. Keep it dark, quiet, and cool. Consider using blackout curtains or an eye mask if light is an issue. Earplugs and/or white noise machines can also help if noise is an issue.
Ensure your mattress and pillows are comfortable, especially if you have neck or back pain. Remove obvious distractions – for example, if checking the clock in the middle of the night makes you anxious, turn the clock away. We always suggest keeping your phone in airplane mode and another room so you aren’t disturbed throughout the night.
Avoid Stimulants and Alcohol in the Evening
Caffeine can affect your body for 6-8 hours, so it’s best to cut off coffee/tea or energy drinks by noon to avoid late caffeine issues. Nicotine is also a stimulant, so it’s best to avoid tobacco or nicotine products close to bedtime. While alcohol might make you drowsy at first, it disrupts your sleep and REM cycles and can cause more awakenings later in the night – so having a nightcap is not a good idea for optimizing sleep quality.
Skip Heavy Meals and Excess Fluids Before Bed
Eating a large or spicy meal late at night can cause indigestion that interferes with sleep. Finish dinner a few hours before bed and avoid those enticing light late snacks. We suggest you reduce how much water or other fluids you drink in the last couple of hours before bed to minimize trips to the bathroom at night.
Only Use Your Bed for Sleep (and Rest)
It’s tempting to lounge in bed to watch TV or scroll on your phone, but this can confuse your brain. You want your brain to associate your bed with sleeping, not with entertainment or stress. If you’re unable to sleep after ~20-30 minutes in bed, it’s better to get up, go to another dimly lit room, and do a quiet activity (like reading), then return to bed when you feel more drowsy.
This process is part of stimulus control therapy for insomnia – breaking the link between the bed and wakefulness. Consistently implementing these sleep hygiene practices can lead to noticeable improvements in your sleep quality over time.
Many TBI survivors find that having structure and routine in their day helps their sleep and other symptoms. It might help to keep a sleep journal to track which habits make a difference. While these changes may not solve severe sleep disorders alone, they lay an essential foundation.
Cognitive Behavioral Therapy for Insomnia (CBT-i)
When simple lifestyle changes aren’t enough to conquer insomnia, Cognitive Behavioral Therapy for Insomnia, or CBT-i, is a highly effective next step to take. CBT-i is a structured, short-term therapy specifically designed to tackle chronic insomnia. It helps you identify and change the thoughts and behaviors perpetuating your sleep problems.
Unlike general talk therapy, CBT-i is very focused on sleep. With CBT-i, you will work with a therapist (or sometimes through guided self-help via web-based apps) on strategies to help you maximize your sleep quality.
Here are a few factors that CBT-i can help you with:
Sleep Education
Learning about sleep cycles and the amount of sleep you realistically need can correct false beliefs (for example, “I must get 8 hours or I’ll never function” – which causes anxiety). Understanding that waking up at night can be normal, or that you might survive fine on 7 hours, can reduce some pressure and ease your mind on sleep.
Stimulus Control
As mentioned, this involves using the bed only for sleep and creating strong mental associations between bed and sleepiness. It also teaches you to go to bed only when sleepy and get out of bed when you can’t sleep, which retrains your body and brain over time.
Sleep Restriction (Scheduling)
This sounds counterintuitive, but a CBT-i therapist might initially have you limit your time in bed to the actual amount of sleep you’re getting (for example, only 6 hours) and gradually increase it as your sleep efficiency improves. When applied carefully, this approach builds a strong drive to sleep through the night to avoid excessive daytime sleepiness.
Cognitive Techniques
Many people living with insomnia have anxiety and racing thoughts at night (“sleep performance anxiety”). CBT-i helps you challenge unhelpful thoughts (like catastrophizing the consequences of a poor night’s sleep) and teaches you to use relaxation techniques when you can’t sleep. Examples of these techniques might include deep breathing, progressive muscle relaxation, or mindfulness exercises.
Improving Your Sleep Environment & Routine
Studies show CBT-i can significantly shorten the time it takes to fall asleep, reduce nighttime awakenings, and improve sleep quality for people with insomnia. More importantly, CBT-i can achieve great results without medication, which may not always have the intended effect of improving sleep.
The American College of Physicians recommends CBT-i as the first-line treatment for chronic insomnia before sleeping pills because of its effectiveness and ability to produce lasting benefits. For TBI patients, CBT-i can be very useful, especially if your primary issue is insomnia and anxiety around sleep.
*Clinical Note: If pain or other medical issues drive your insomnia symptoms, treatment must encompass all of them in tandem. With that stated, CBT-i can still help you control your response to those discomforts at night.
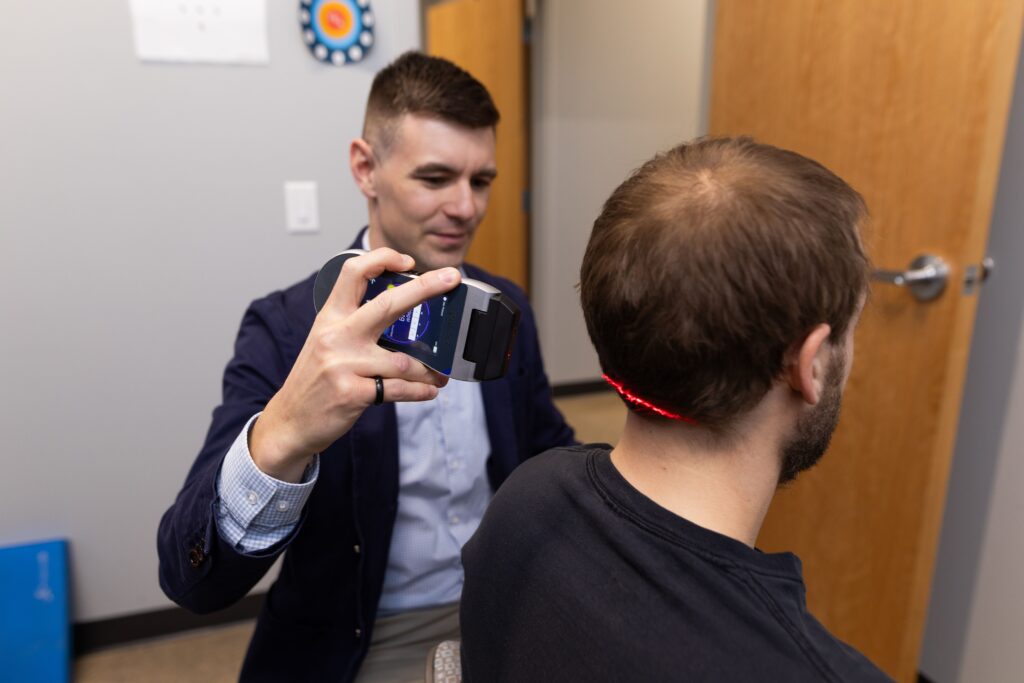
Low-Level Laser Therapy (Photobiomodulation)
Light is one of the most powerful regulators of biological function. While natural light is helpful for circadian regulation, there’s an even more targeted tool showing promise in post-TBI recovery: low-level laser therapy (LLLT), a specific form of photobiomodulation (PBM).
One of the leading technologies in this area comes from Erchonia, whose FDA-cleared low-level lasers emit specific wavelengths of light that influence healing at the cellular level.
Unlike light therapy boxes that affect the eyes, Erchonia’s low-level laser therapy penetrates deep into the tissue. These photons deliver high amounts of energy that is absorbed by the mitochondria to optimize cellular healing. These wavelengths of energy stimulate the mitochondrial electron transport chain, optimizing ATP (adenosine triphosphate) production, the primary fuel for all cellular activities.
This process matters after a brain injury because the brain often suffers from mitochondrial dysfunction, oxidative stress, and impaired cellular communication following a TBI. These altered cellular pathways contribute to symptoms like fatigue, brain fog, inflammation, and poor sleep.
Peer-reviewed studies confirm that LLLT improves mitochondrial function, reduces neuroinflammation, and enhances neuroplasticity. Since Erchonia has 22 FDA clearances for LLLT use on chronic pain and musculoskeletal issues, it’s a no-brainer for us to partner with them.
At The Neural Connection, we use Erchonia’s lasers as part of our integrative strategy. It’s non-invasive, safe, and synergizes with integrative therapies like neuro-rehabilitation and autonomic balancing. Patients often report reduced fatigue, fewer headaches, and more restorative sleep.
Curious whether low-level laser therapy might be a good fit for your recovery? Contact us at The Neural Connection for a free consultation.
We’ll design a plan to meet your brain and body’s unique needs.
Sleep Medications and Supplements
We suggest exploring medications or supplements when non-pharmacological methods aren’t providing enough relief. It’s important to use these judiciously, as they can be helpful in the short-term or severe cases, but they often don’t solve the root problem alone.
Here’s an overview of common sleep medications and supplement options:
Prescription Sleep Medications
Your medical doctors might prescribe sleep aids such as Zolpidem (Ambien), Trazodone, or Benzodiazepine medications for short-term use to improve sleep.
In some TBI cases with severe insomnia, these medications can help ensure the patient gets some rest, which is crucial for healing. Additionally, certain antidepressants (like Amitriptyline or Mirtazapine) may be used off-label at night for their sedating effects to improve sleep.
On the other hand, using stimulants or wakefulness-promoting agents like Modafinil or Methylphenidate may help you stay awake and engaged during the day but can be an issue for people with hypersomnia symptoms at night.
Note that each of these medications targets a symptom, but none cure TBI-related sleep disturbances. They also often come with side effects such as next-day drowsiness, risk of dependency (especially some sedatives), or interactions with other TBI medications.
Generally, physicians aim to use the lowest effective dose for the shortest period necessary while concurrently addressing underlying issues via therapy and lifestyle changes. Sleep habits will always come into play during these stages of finding treatment.
Over-the-Counter Aids and Natural Supplements
Many people are interested in alternatives to prescription drugs to avoid heavy side effects.
Melatonin
Supplements with Melatonin are often a popular choice, especially for circadian rhythm issues and mild insomnia. Taking Melatonin in the evening (usually 1–5 mg about an hour before bed, under a doctor’s guidance) can help cue your body that it’s time to sleep.
Research indicates that Melatonin can improve sleep quality and increase total sleep time in TBI patients. It essentially compensates for the lower Melatonin your brain might be producing, which may be an outcome of the TBI.
Valerian Root
Another common supplement is valerian root, an herbal remedy. Many drink it as tea or consume it in capsules to promote further relaxation and better sleep. While valerian has been used for primary insomnia, its effectiveness, specifically in TBI patients, is not well-studied, although it may help some individuals as a mild sleep aid.
Other Supplements
Other supplements occasionally considered include magnesium threonate (which can have calming effects and crosses the blood-brain barrier), L-theanine (an amino acid promoting relaxation, commonly found in tea), or CBD/CBN/CBG oil (cannabidiol, which some find improves sleep and anxiety – legality and effects vary).
*Clinical Note: It’s crucial to discuss any supplements with your healthcare provider. Sadly, “natural” doesn’t always mean safe (for example, herbs can interact with medications or affect brain chemistry). Sleep problems after a TBI can be multifactorial, so make sure your providers know what you’re taking.
Treating Specific Sleep Disorders via Medical Devices
If a specific condition like sleep apnea is diagnosed (often via a polysomnography (PSG) sleep study), the treatment might involve devices like CPAP (Continuous Positive Airway Pressure) to keep the airway open at night, or dental appliances to adjust jaw position.
Treating sleep apnea can dramatically improve sleep quality and reduce health risks. Similarly, if restless legs syndrome or periodic limb movement disorder is present, medications like Gabapentin or dopamine agonists can be scripted for use. The key is that a thorough evaluation should guide targeted treatments.
*Be advised: Medical supervision, whether medications or supplements, medical devices, or various sleep therapies, is critical for short and long-term success.
Why We’re Different at The Neural Connection…
At The Neural Connection, we focus on treating the problem. The ideal scenario is to use medications as a bridge to get you sleeping better while concurrently working on the therapies and lifestyle adjustments that address the root causes. In our experience, many patients can taper off the meds once their brains have recovered enough and their routines are optimized.
Always follow your doctor’s instructions for usage and report any side effects. Never mix sleep medications with alcohol or other sedatives, and keep them safe, as some (like certain sleeping pills) can be habit-forming if misused. Sleep problems after a TBI are rarely fixed with medications, but they can often help in the short term.
At The Neural Connection, we don’t prescribe medications directly, but our team will coordinate with your physicians and medical providers if medication is warranted.
Because of this, we take an integrative approach – which means if you need a sleep med to get through a rough patch, we support that, but we will also work on complementary therapies to reduce your reliance on meds in the long run.
Our ultimate goal is to help you sleep well naturally…
Why Sleep Medications and Basic Therapy Alone May Not Be Enough
By now, it’s clear that sleep problems after a TBI are rarely an isolated issue. They’re often a combination of other neurological, physical, and psychological issues underlying the injuries.
Many patients with post-TBI sleep disturbances are also coping with headaches, dizziness, fatigue, cognitive impairments (like memory and attention problems), depression, and anxiety, all at the same time. Because these symptoms often feed into each other, treating just one piece of the puzzle will usually yield limited results.
Let’s consider an example:
Suppose you have a persistent post-concussion headache and resulting neck pain, plus insomnia. Suppose your doctor only addresses your insomnia by giving you sleeping pills. In that case, you might sleep a bit more – but the untreated headache pain still wakes you up at 3 AM, or the underlying brain inflammation still leaves you feeling unrefreshed. You haven’t solved the problem yet…
Conversely, if a doctor only treats the headache with painkillers, you might still be too anxious and wired at night to see the benefits. While the pain has decreased, your sleep is still an issue, which can further cause more pain now that the brain hasn’t had time to recover.
You may improve in both cases, but the core issues remain, hampering full recovery.
As you can see, a comprehensive, personalized, and integrative approach is essential for proper healing from a TBI. Cookie-cut approaches may work in other areas of medicine, but traumatic brain injuries require far more consideration and understanding.
This approach means looking at you as a whole person – not just prescribing a sleep aid or doing a bit of counseling in isolation based on symptoms. Traditional therapy for insomnia (like CBT-i) is great, and medications can help temporarily, but if your sleep problems are symptoms of deeper issues from the TBI, then we have to treat those dysfunctions, too.
And this is really where the rubber meets the road for finding personalized and integrative care.

The Neural Connection’s Integrative Approach to Healing Your Brain After TBI
At The Neural Connection, we believe empowering patients through education and integrative therapies is the key to overcoming post-TBI challenges, symptoms, and sleep disturbances. Our clinic’s philosophy is patient-centered and based on a holistic approach to care: We focus on addressing the structural, neurological, and metabolic components of your health to support your recovery.
In practice, this means when a patient comes to us with TBI-related issues (sleep problems, cognitive symptoms, dizziness, pain, etc.), we design a comprehensive and personalized treatment program tailored to all aspects of their condition.
This personalization is where our program differs from the conventional approaches to care. We don’t see your sleep problems in a vacuum. To improve your sleep, we must improve global brain health, hormonal imbalances, pain levels, altered stress responses, and help optimize your daily routine.
It’s a big task, but it’s achievable with the right team, personalized approach, and integrative therapies…
Just look at our 100+ Google Reviews to see for yourself!
Research studies and our clinical experience have shown that patients who undergo comprehensive brain injury rehabilitation often report significant improvements in sleep as their other symptoms improve. By treating root causes – for example, doing therapies that restore normal blood flow to the brain and reduce neuroinflammation – you might find that your insomnia or hypersomnia naturally diminishes. Sleep problems after a TBI don’t have to be your new normal.
To put it simply: Quality sleep is a cornerstone of brain injury recovery, and conversely, quality recovery can help to restore healthy sleep. You need both sides of that coin. If you haven’t found solutions for your sleep problems, you may need a more integrative approach to tackle these interconnected issues.
Comprehensive Evaluation and Personalized Plan
We always start with a thorough neurological and orthopedic evaluation to understand your unique situation. This isn’t a rushed 15-minute appointment – it’s a 90-minute deep dive into your health history and current challenges, paired with a comprehensive, in-depth evaluation.
One of our highly trained providers will sit down with you to review details like:
- What was the nature of your brain injury (or injuries)?
- What symptoms are you experiencing (not just sleep issues, but everything – headaches, dizziness, mood changes, cognitive difficulties, etc.)?
- What treatments have you tried, and what helped or didn’t?
- We also review any relevant medical records, such as hospital reports or imaging (e.g., MRI results) you may have.
In many cases, we may conduct or coordinate additional tests to gather objective data.
An In-Depth Bedside Neurological Examination
This examination will assess reflexes, balance, coordination, visual and vestibular function, and other neurologically-based functions to spot any neurological deficits contributing to your symptoms.
Sleep Assessment
If not already done, we’ll evaluate your sleep patterns. Sometimes, this is through sleep questionnaires or diaries. In certain cases, we might refer you for a sleep study (polysomnography or a home sleep test) if sleep apnea or other specific disorder is suspected. Tracking your sleep with wearable devices or apps can also give us insights to use. Sleep problems after a TBI are often an indication of a multitude of factors, which is why they require further investigation.
Objective Videonystagmography Testing
By quantifying visual and vestibular markers, we can determine the function and integrity of these systems to see what may be causing symptoms of dizziness, visual pain, headaches, and brain fog.
Functional Diagnostic Imaging
While we don’t necessarily do diagnostic imaging on-site, we collaborate with neurologists and radiologists if needed. If you haven’t had a recent MRI of your brain (and cervical spine, if neck injury is relevant), we may recommend getting one to rule out any structural issues that need attention (like, say, an unhealed neck injury or cervical disc contributing to pain).
More advanced imaging or scans can sometimes be helpful in pinpointing functional issues. For example, some specialized clinics (and we can arrange referrals) use qEEG (quantitative EEG) to look at brain wave patterns or PET scans for metabolic activity. These can reveal lingering effects of TBI that routine scans might miss, which can give us more data into your function, not just structure.
Laboratory Tests
Because of the metabolic aspect of our integrative model, we often check specific lab values. For instance, blood tests for hormone levels (like thyroid, adrenal hormones, sex hormones, and melatonin metabolites) can uncover imbalances. We often check for nutritional deficiencies (like low vitamin D or B12) or markers of inflammation (like ESR, CRP, and homocysteine), as they can affect fatigue levels and sleep quality. Suppose we suspect something like growth hormone deficiency (which can happen after pituitary injuries in TBI) or underlying gut dysfunction. In that case, we also have tests to assess these factors too.
This comprehensive workup helps us assemble all the puzzle pieces to help you find answers and get relief. It’s not uncommon for us to discover contributing factors that were missed before – for example, a subtle vestibular issue from the injury that’s causing dizziness and contributing to anxiety or a thyroid imbalance making you tired. With a complete picture in hand, we create a personalized treatment plan specific to you and your brain.
Your personalized plan will target the specific areas of dysfunction identified.
For instance, if we find evidence of autonomic nervous system overdrive and anxiety, part of the plan will focus on calming techniques and potentially utilizing neurofeedback.
If neck muscle tension and headaches are a big issue, we’ll emphasize manual therapy, visual and vestibular treatment, and home exercises to manage pain.
Our goal is to address whatever your brain and body require to heal.
Integrative Therapies – Treating the Whole Person
As you can see, our treatment programs at The Neural Connection typically involve a blend of therapies addressing the structural, neurological, and metabolic aspects of your health.
Here are some key components and how they help, especially concerning sleep:
Neurological Rehabilitation
Neurological rehabilitation can include various forms of treatment like cognitive therapy and even neurofeedback.
Cognitive therapy involves exercises and training to improve brain function – memory games, attention tasks, coordination drills, etc. It helps rebuild neural connections and improve neurovascular coupling. For example, working on attention and reaction time tasks can indirectly help sleep by reducing brain fog and mental fatigue, so you’re more naturally tired at night.
Neurofeedback is a technique where you train your brainwaves into healthier patterns using real-time qEEG feedback. It’s shown promise in reducing insomnia by teaching the brain to shift into more relaxed states at night.
If indicated, we collaborate with our clinical partners to perform neurofeedback to help regulate your brain’s activity. Sleep problems after a TBI can often be treated with brain-based therapies and integrative approaches.
Physical and Structural Therapy
Many TBI patients benefit from functional therapies like physical therapy and chiropractic care to address the physical injuries that come with brain injury (like whiplash, vestibular problems, and balance issues).
How does this relate to sleep?
As we’ve previously discussed, relieving chronic pain and muscle tension with manual therapies (massage, myofascial release, gentle chiropractic adjustments, etc.) can significantly improve your comfort and ability to sleep. This is crucial if neck pain or headaches have been waking you up.
We also often incorporate neuromuscular therapy – techniques that combine movement and muscle work to improve coordination and reduce pain. These therapies might include exercises for balance and posture, which can calm down the nervous system.
After these sessions, patients often report feeling relaxed and sometimes pleasantly tired – a good recipe for better sleep at night. By improving your body’s alignment and easing discomfort, we remove physical barriers to sleep.
Vision and Vestibular Therapy
TBIs frequently cause vision disturbances or inner ear (vestibular) issues contributing to dizziness or eye strain. These issues can directly and indirectly affect sleep by causing symptoms that keep you up at night.
Constant dizziness or visual strain can be very stressful and fatiguing. Our therapists use vision therapy (like eye-tracking exercises, Brock strings, alphanumerics, and Blaze pod reaction time programs) to rehabilitate your ocular function.
We also use vestibular therapy to help improve your balance, spatial orientation, and coordination.
As you regain these functions, the reduction in dizziness and motion-triggered nausea often leads to reduced anxiety and better overall relaxation – again feeding into better sleep at night.
Autonomic Assessments and Training
Autonomic imbalances are often seen with TBIs, with patients usually stuck in fight or flight mode. Because of this, utilize techniques in the clinic to train your body to enter the “rest and digest” mode. We commonly deploy Vagal Nerve Stimulation (VNS) as a therapy to help you get into an optimized parasympathetic state to balance your autonomics.
These clinical approaches may involve biofeedback sessions, where you learn to control your heart rate or breathing patterns with feedback from sensors and HR monitors. We also teach breathing exercises like diaphragmatic breathing, 4-7-8 breathing, and mindfulness meditation practices that you can do daily.
Over time, these practices can lower your baseline stress levels, which can help to optimize sleep and recovery. Many patients find that as they master these techniques, they fall asleep faster and wake up less often because their bodies aren’t consistently in constant fight or flight mode.
Nutritional and Metabolic Support
Diet and nutrition are pillars of healing that we consistently find overlooked by other providers. Our providers are all trained in nutrition and functional medicine to provide specific nutritional guidelines to ensure you’re fueling your brain recovery.
We focus on research-backed approaches to care by deploying a high-fiber, anti-inflammatory, balanced diet – rich in omega-3 fatty acids, antioxidants, healthy fats, and adequate protein.
Specific diets (like a Mediterranean diet or a modified ketogenic diet) can help improve brain health for particular patients, depending on their needs and previous history. We also address underlying gut health because a healthy gut can reduce inflammation and enhance neurotransmitter production (You produce 70-90% of your body’s serotonin in the gut!).
Suppose your evaluation showed certain nutritional deficiencies or needs you’re not getting through your diet. In that case, we may advise supplements like vitamin D (low levels can cause fatigue and poor mood), B vitamins (for energy metabolism), magnesium threonate (helps muscle relaxation and sleep, crossing the blood-brain barrier), or omega-3s (for brain repair and regulating inflammation).
Any hormone deficiencies discovered (like low growth hormone or low thyroid) would also be co-managed with an endocrinologist to correct, as fixing those can boost energy and sleep quality.
As you can see, our providers at The Neural Connection will treat you from the inside to ensure your body has the building blocks to heal and recover.
Psychological Support and Counseling
At The Neural Connection, we work very closely with compassionate psychologists, psychiatrists, and mental health experts who have vast experience with brain injuries and concussions.
Dealing with a TBI and its aftermath can be emotionally taxing. We aim to provide a space for patients to process trauma (emotional trauma from the injury event), cope with changes in life roles, and develop resilience. Techniques from cognitive-behavioral therapy (CBT) are often used to help manage the emotional waterfall that occurs after these injuries.
During your program at The Neural Connection, you will likely engage in a combination of these therapies each week.
For example, you might have a schedule where each day you do some aerobic exercise (to pump up neurovascular coupling), cognitive training, then a massage or myofascial release session, guided meditation, or mindfulness practices. It’s all tailored to you and what you need, not just another cookie-cutter approach.
It’s a full-body, full-mind approach.
More importantly, all these therapies are coordinated for you – our team meets daily to discuss your progress and tweak the plan as needed. If something isn’t helping or you find a particular therapy especially beneficial, we adjust accordingly.
Your feedback is valued; after all, this is patient-centered care…
By treating the multiple dimensions of your condition, we aim to achieve synergy in healing. Many patients report improvements in their targeted symptoms and overall well-being – they have more energy, clearer thinking, and better sleep. Sleep problems after a TBI can also improve with the right therapies.
In fact, by the time we’ve addressed pain, stress, hormonal balance, and brain function, patients often find that sleep falls into place naturally. It’s not magic; it’s the result of the brain and body recovering and regaining balance.
Ongoing Support and Recovery
Our commitment to your recovery doesn’t end when the intensive phase of therapy ends. We know that recovery from a TBI is a journey, and there will be ups and downs along the way.
Sleep, in particular, can still have the occasional hard night even when you’re much improved (everyone has occasional stress or flare-ups).
That’s why our work at The Neural Connection emphasizes education and self-management strategies. When you finish a neuro-intensive program with us, you’ll have a toolkit of techniques you can continue at home to help you continue to heal and improve. We also provide detailed guidance as part of your discharge planning.
We also schedule follow-ups to check on you and make minor tweaks to your home program. If new issues arise or old ones threaten to return, we can adjust your plan, coordinate care with your providers, and find ways to keep you moving forward.
We care and want you to live the life you know you’re meant to live…
Patients often choose to do periodic in-office follow-up sessions (for example, coming in once a month for structural work and consult or doing a recovery day with passive modalities) to stay on track.
Our goal is to make you as independent and empowered as possible. You’ll know how to maintain good sleep hygiene, how to apply cognitive strategies if insomnia creeps back, and when to seek help if something changes.
Above all, we approach each patient with compassion and understanding at The Neural Connection. We know how deeply frustrating sleep problems after a TBI can be. We’ve seen the exhaustion on people’s faces when they arrive, and thankfully, we’ve seen the relief after treatment when they report finally getting a full night’s sleep again.
It’s incredibly rewarding for us to help someone turn that corner!
If you’re struggling with sleep after a brain injury, we invite you to take the next step toward recovery.
Click the link below for a free phone consultation with our team!
We’ll listen to your story, answer your questions, and help you understand what might be happening and how our integrative approach could help you. And finding answers for your sleep problems after a TBI is at the top of our list.
There is hope for improvement and you don’t have to navigate it alone!
Start Your Healing Journey with Better Sleep
If you or a loved one is suffering from sleepless nights, foggy days, or relentless fatigue after a concussion or TBI, reach out to The Neural Connection for a free consultation!
Our compassionate doctors will work with you one-on-one to create a plan that empowers you to regain control of your sleep and your life.
Whether you’re dealing with insomnia, hypersomnia, or any other TBI-related issue, we are ready to support you with proven therapies and a caring approach.
Remember: You are not alone in this journey; recovery is possible. Many before you have walked this road and come out the other side living whole, rested lives.
With the right help and a personalized integrative treatment plan specific to you, you can find relief, too. Don’t wait to get the help you need – better sleep and better healing can start today.
Contact us at The Neural Connection to schedule your free consultation and take the first step toward reclaiming your nights and rebuilding your health.
We look forward to partnering with you on your path to recovery and seeing you thrive again!
To book your free consultation or to learn more about TNC’s integrative TBI programs, click the link below!

