Neck Pain After a Concussion
Neck pain after a concussion is one of the more common symptoms that can show up minutes, hours, weeks, or months after the injury. It is especially common following a whiplash injury and can present as sharp, stiff, dull, or anything in between. We often hear about a vice grip at the top of the neck, right below the base of the skull.
Recent research has pointed to the fact that whiplash injuries should be treated as concussions because there is such tremendous overlap in symptoms. When you consider the mechanism of injury, it also makes sense if an impact is strong enough to damage soft tissues in the neck; it is strong enough to shake the brain inside the skull. In the picture below, the left side is concussion symptoms and the right side is whiplash symptoms.

Photo Credit: Complete Concussions
As a general rule, if the neck pain is present within 2 weeks of the concussion and progressively improves with muscle-based therapies, it’s likely to resolve on its own with time, rest, and recovery. If it persists beyond 2 weeks and doesn’t respond to anything, it’s likely coming from post-concussion syndrome (PCS).
One of the problems people run into when finding relief for neck pain after a concussion is identifying the source, or sources. Due to the complex nature of concussions, there are often several different sources, all contributing at varying times in different environments. This article will help you understand why this may be happening.
Later on, we’ll cover:
-Different causes of neck pain after a concussion
-How to diagnose neck pain after a concussion
-Treatment options
-Tips for home management
If you have questions about concussion recovery, click here to schedule a complimentary consultation with one of our doctors. We’ve treated hundreds of complex neurologic cases and can help piece together the missing pieces in your recovery.
*Note: The information provided in this article is for educational purposes only and does not constitute a doctor-patient relationship. Patients should consult their medical provider or primary care physician before trying any remedies or therapies at home.
What Causes Neck Pain after a Concussion?
Identifying the exact source of neck pain after a concussion is not always as straightforward as we’d like. In a perfect world, we can point to and treat a single point that was impacted. In practice, we often find concussions tend to create neck pain from several locations at different times.
For example, if the systems that help your eyes move are injured in a concussion, the brain will compensate for the inability to hold your eyes steady by ramping up the tension in your neck. This helps keep the eyes on target and reduces the chances of something dangerous occurring due to a lack of vision. We see a similar reflex occur in injuries involving the vestibular system. In short, when the eyes can’t hold steady, the neck often tenses up to hold the head steady.
There is also physical damage to the soft tissues in the neck. Whiplash is associated with rapid acceleration/deceleration, which occurs too quickly for the neck muscles to contract and brace for impact. This can affect the ligaments and soft tissues of the neck, which are there for support. When these support systems break, the muscles often pick up the slack. There are other forms of soft tissue involvement described in a later section.
Lastly, autonomic symptoms can underlie other forms of dysfunction and make minor problems into big problems. Autonomic dysfunction, which is easily understood as a balance between stress responses and relaxation responses, is commonly skewed toward stress following a concussion. This is especially true if multiple systems are involved. When the autonomic system is stuck in “fight or flight” mode, any dysfunction present in other systems is ramped up because of decreased blood flow. More on that later.
Now, we’ll examine each system and explain why it causes neck pain. We’ll also discuss types of therapy that work well with each system.
Structural Damage to the Cervical Spine (Neck)
Multiple issues can stem from a concussion. Things like disc herniation, ligament sprain, and muscular tears are all in play following a concussion. These are especially common after a whiplash injury but can occur after other types of concussions as well.
If you have any pre-existing issues, like old injuries, scoliosis, or disc issues, a new concussion may worsen old symptoms. If you suspect new injuries due to new symptoms, consult a medical provider immediately and rule out any new issues. Signs you should see a doctor immediately are numbness and tingling down into the arms, weakness, new dizziness, or loss of bladder/bowel control.

Photo Credit: VeryWell Health
When You Should Seek Help for Neck Pain After a Concussion
If you sustain a concussion and you have any of the following symptoms, you may have damaged some aspect of the cervical spine.
- Stabbing pain occurs during specific movements or remains present most of the time.
- Progressively worse neck pain that spans more than 2 weeks.
- Limited, painful range of motion.
- Loss of strength in arms and fingers.
Initially, you may seek out a physical exam to assess the damage. If the provider can’t confirm an exact source of injury, or if there are red flags that point to structural damage, they may refer out for an image of some kind.
X-rays help rule out broken bones and other injuries. CT scans are often helpful because they provide more detail for blood vessels and soft tissues. MRI imaging is the most beneficial, showing discs, soft tissues, and bones together in a single image.
As a general rule, if your imaging is precise and you’re still having symptoms 2 weeks following the injury, you’re likely dealing with post-concussion syndrome, and the issues are “functional” in nature. This means it’s not broken; it’s just not working all the way. This is when you start looking outside of the neck for relief.
Autonomic Nervous System (ANS) Dysfunction
We often refer to the autonomic system as the “automatic system” because it handles processes you don’t think about. This nervous system branch includes blood pressure, heart rate, breathing, and digestion.
The ANS has two parts, each acting in combination with the other. These branches are called the “sympathetic” (commonly known as the “fight or flight” branch) and the parasympathetic (widely known as the “rest and digest” branch)anch.
These two systems act like a see-saw, with one typically more active than the other. Healthy people have a balance in this relationship, where one end of the see-saw isn’t touching the ground. Adding in ongoing head and neck issues after a concussion adds weight to the “fight or flight” side, eventually leading to something called “dysautonomia.”
Dysautonomia is a catch-all term for an imbalance between these 2 branches of the ANS. When someone has a concussion and experiences prolonged activation of the fight-or-flight system, the body responds by preparing itself for something dangerous. This means lots of adrenaline, cortisol (your body’s stress hormone), and muscle tension. These chemicals and excessive tension easily make a tight neck feel worse. To make matters worse, issues caused by the ANS don’t respond well to traditional therapies like chiropractic and massage.

Anxiety After a Concussion
Anxiety is also a common complaint following a concussion. The overactivation of the sympathetic (fight or flight) system leads to a chemical environment that can either cause anxiety outright or accelerate pre-existing anxiety. This further creates muscle tension that is resistant to therapy.
It’s common to hear about neck pain that doesn’t respond to anything. It may feel good for an hour but come back the same or sometimes worse than before. This is an excellent indicator that the pain is coming from something other than the muscles/bones of the neck.
One of the most common sources of this stubborn neck pain is something called a “sensory mismatch.” I always tell a story about a patient to illustrate this point.
A woman came into the clinic after getting rear-ended by a pickup truck. She was a slight woman driving a vintage sports car. If you’ve ever been inside old sports cars, some don’t have a headrest. Getting rear-ended in a car seat that doesn’t have anything to stop your head is a recipe for intense whiplash.
She came in with symptoms of headache, neck pain, and nausea so intense it made her throw up several times a day. She had been to a chiropractor 3x/week for 3 months before coming to see us. After examining her, I noticed her head was bobbing up and down, consistent with the complaint of “feeling like I’m on a boat all the time.” I asked her if she felt it, and she said no. I pulled up a mirror and showed her what was happening, but she couldn’t believe it.
Her neck had been so severely whiplashed that even when it was moving, the muscles weren’t sending appropriate input. This lack of input disagreed with the other sensory systems, and the result was nausea so bad she would throw up on repeat every day since the accident. We treated this aspect of her neck while treating the vestibular issues, and it resolved in 2 weeks.
If you have neck pain after a concussion, there is a high likelihood of disagreement between the eyes, neck, and vestibular (balance) systems. This ongoing miscommunication results in a stress response and usually nausea.
If you have questions about concussion recovery, click here to schedule a complimentary consultation with one of our doctors. We’ve treated hundreds of complex neurologic cases and can help piece together the missing pieces in your recovery.
Vision and Vestibular Issues
People don’t realize how connected the eyes and the neck are. Try this. Put your fingers at the location in the picture below. Move your eyes to the extreme left, right, up, and down. You’ll feel the muscles under your fingers gently twitch if you’re in the right spot. These two systems are tightly connected, so you can quickly move your head and eyes to locate things in your environment precisely. It would look strange if you only used your eyes or only turned your head to look around the room. You use both all the time.
With this in mind, it makes sense that if your neck is damaged or sends poor feedback, the brain will tighten these upper neck muscles to compensate. People with this issue will often get terrible headaches in busy visual environments like supermarkets, libraries, or sporting events. It’s especially bad during prolonged screen time.
The other big issue here is the equally tight connection between your visual system and your vestibular system. Try this. Look at something off in the distance and move your head in every way possible. Notice how you’re easily able to hold your focus on that object? This is called the “vestibulo-ocular reflex”. It allows animals and humans to move quickly and maintain a central vision of objects. In ancient times, it helped people move around and see potential danger on the horizon.

Photo Credit: Strabismus World
Another way of thinking about the vestibular system is comparing it to the axle in a car. If the axle is bent, it will steer off the road if you let go of the steering wheel. We cover up the eyes to assess vestibular conditions and see how they drift. If they drift, there are commonly deficits in how the eyes can move. Think about how hard driving a car with a bent axle would be. You’re constantly steering it back to the center, which affects how you can drive.
When the brain knows a faulty vestibular system is pulling the eyes, it will compensate by locking up the cervical muscles to maintain focus on the room around you. This backup reflex helps you maintain spatial awareness, but it comes at a price. The price is neck tension that doesn’t go away when you work the muscles.
Altered Pain Processing
If you’ve ever heard the phrase “pain is all mental,” it’s not all wrong. It’s also not all right. Pain is a complex experience that can be affected by several factors. This is why some people seem to have superhuman pain tolerances while others develop chronic pain syndromes. It all has to do with how factors mix together and how your brain interprets that mixture of signals.
Have you ever given yourself a paper cut and not noticed it until you looked down and realized you were bleeding? When you see the cut, your brain immediately identifies this as bad, and you feel all the pain rush in. Your perception of pain has much to do with how intense it is. If you think your neck is permanently damaged, or someone told you the curve isn’t right, and that’s why you have pain, you can form beliefs about neck pain that intensify it. It’s a process known as “no-cebo”. It’s like a placebo, but instead of believing something fake is accurate, you believe something is real when it’s not.
Other ways pain can become intensified is through damage to areas of the brain that relay pain to the brain. One is called the thalamus, and it’s located deep within the brain. Ongoing inflammation or injuries that involve a lot of twisting motion can damage these relay centers. This results in a distorted perception of pain that can become larger or more intense than the original signal.
Lastly, you can damage the areas in your brain that produce natural pain-killing chemicals. Whiplash injuries often affect an area at the top of the brainstem called the midbrain. This area controls many things, such as vertical eye movements and looking near to far. It also controls the natural production of serotonin in the brain via an area called the periaqueductal grey. This area makes pain-killing chemicals, and when it’s injured, it can lose that ability, which results in an augmented sense of pain.
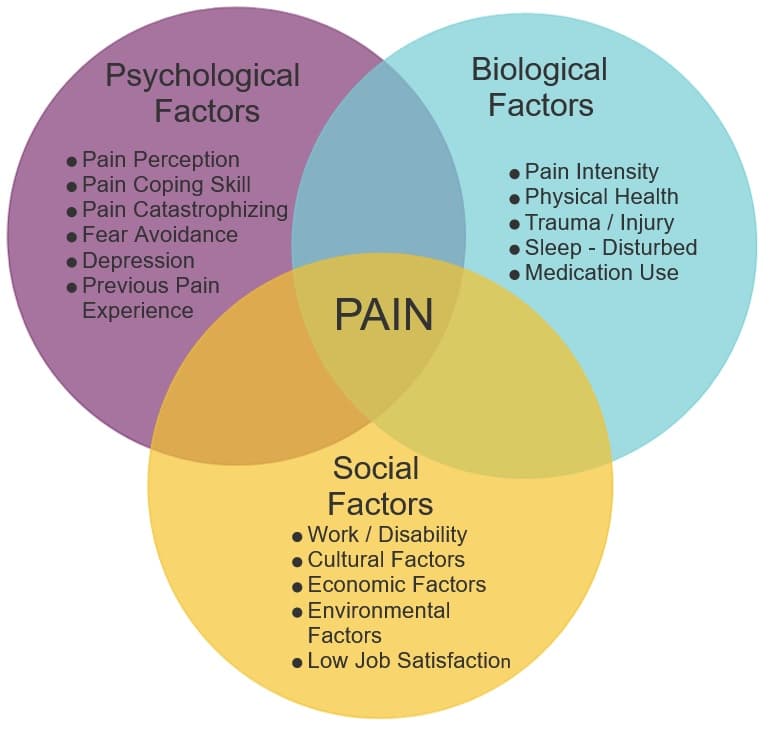
Photo Credit: Chiro.org
Prolonged Compensation
It’s common for concussions to create all sorts of weird postural compensations. For example, advanced neurologic disease like Parkinson’s disease is commonly associated with a hunched forward posture. One of the reasons this occurs is because vestibular system breaks down and tells the brain the person is falling backwards. This vestibular signal causes a postural compensation that makes the person lean forward so they don’t fall over.
Similar things can occur with a concussion, leading to neck pain. One of the things we check for in our exam is resting head and neck posturing. People will often turn or rotate their heads toward the side of vestibular or cerebellar dysfunction, which gives us valuable clues as to where the damage is and why the neck hurts.
These compensations, while helpful in the diagnostic process, can create ongoing neck pain because the head is in a position it’s not supposed to be in for a long time. It’s the same reason why sitting at a desk with poor posture for 8 hours daily will give you a headache. But with compensations, people often don’t know they’re doing it, so it’s harder to correct in real-time.
Treating Concussion Headaches
I’m sure by now you realize what a challenge effectively treating concussion headaches can be. There are many combinations of causes and an ever-greater number of specialists who may or may not be able to help. This section will review all the options and help you decide what options are best for you.
A Note on Medications.
A concussion will often land you in a doctor’s office, making sure nothing is outright broken in your head. While this is a good first point of contact and the right decision for your safety, understand that the job of a medical provider is not necessarily to improve your quality of life. Their job is to preserve your life.
This is an important distinction because many people will say, “Nothing is broken, so you should be fine.” This can be confusing and emotionally hard to swallow when you know something is off. They’re looking for things that can be treated with medications, surgery, or injections most of the time. On that note, there are currently no FDA-approved medications to treat concussions. Furthermore, many headaches, even if they’re not truly migraine, will get medicated with drugs that have many well-documented side effects, many of which you may be struggling to find relief for.
For example, many people will get prescribed the medication sumatriptan for a post-concussion headache that looks like a migraine. Some of the listed side effects of this medication are “headache, dizziness, nausea, and confusion.” The point is, be weary of relying on medication to resolve your post-concussion issues. They are typically unaffected by post-concussion symptoms, and if you’re not dealing with genuine, genetic migraine, they will likely make your other concussion symptoms worse.
Treating Concussion Neck Pain Holistically
We’ve seen hundreds, if not thousands of post-concussion cases in our career at The Neural Connection.
Our process starts with a consultation to ensure it’s the right time for this type of treatment. This involves a 30-minute phone call during which one of our doctors will discuss your medical history, what’s worked, what hasn’t, etc. This is important because it allows us to either make the most appropriate referral to something that will help right now or recommend proceeding with an examination.
If the person is a good candidate, they will come in for our initial examination. It starts with a history based on the information provided in the intake. We’ll also review some questionnaire forms to understand emotional status, readiness for change, cognitive function, etc.
Once we grasp the situation well, we jump into our comprehensive battery of tests. We start with a VNG, which allows us to diagnose exactly where the vestibular system is damaged and to what extent. It also allows us to quantify ocular tracking, the ability to follow objects, and several other aspects of the visual system.
We then move to autonomic testing to see whether or not the ANS is causing any of the symptoms. From there, we test the injury’s neck and other orthopedic aspects to see how much physical rehabilitation needs to be integrated into the program. Finally, we perform an entire bedside exam to develop an understanding of any other small detail that might help us pick the right therapies.
From there, if the person is a good candidate for care, we’ll recommend several options. With every option, the goal is to achieve “plasticity.” This is the process of physically re-wiring new pathways into the brain with repetition and gradual increases in intensity. It’s the same process that happens when you’re learning something new. At first, you need a lot of repetition to keep the information, but eventually, you have it so memorized that you no longer need to read it. That’s plasticity at work. Forming new habits works the same way.
To achieve plasticity, patients often elect to use our intensive model. Out-of-town patients come for a week and make three appointments a day. They are then given an at-home therapy program to finish cementing the plasticity process. The intense nature of the program jump-starts the process of creating the proteins necessary for plasticity. Then, with enough repetition and intensity at home, the system requires a new pathway. This allows our therapy to continually provide lasting relief into the future.
Local patients typically elect for a slower process known as the 21-day intensive. It’s the same number of appointments, just spread out over 3 weeks instead of 1. Our 100+ 5-star reviews are primarily from people who did intensive programs, which you can read here.
Steps to an Intensive Program
Each appointment in an intensive will generally follow the same series of events listed below.
Preparation
Patients will warm up for 5-10 minutes on our stationary bike. This helps provide the brain with oxygen and prepares the autonomic system for work. It also helps produce vital chemicals that allow plasticity to occur. We then begin with low-level laser therapy and regular compression boots. Laser therapy helps create more energy in the tissue we need to work, and the boots help return blood to circulation. We’ll conclude this initial process with some vagal nerve stimulation to ensure the entire system has enough room for rehab.
We’ll typically address underlying autonomic rehab before beginning the second rehab phase, which involves individual system work.

Individual System Rehab
Once the system is prepared for rehab, the first step is vestibular rehab. Think of the vestibular system as the axle of a car. You can’t drive it very fast if the car constantly pulls to one side. Once the system has been integrated, we can move to specific ocular and neck rehab forms. This often comes in the form of eye-tracking exercises, gaze stability work, saccades, and laser-guided cervical proprioception training, to name a few.
Once these individual systems have had a chance to improve, we move into the 3rd phase of care: Integration exercises.

Integration Exercises.
This is where the rehab begins to stick. Once each system has had a chance to improve, we move into exercises that work all systems simultaneously. Think of it like members of an orchestra. The music won’t sound perfect if the entire band only practices their parts individually. The group needs time to play together to sound good. This is where our program earns its keep. Integrating everything into exercises that work simultaneously allows the system to recalibrate and work as a whole unit. With the siloed nature of concussion care, this aspect is crucial for long-lasting results. Once we get someone here, the focus shifts to progression.
Progression
The final aspect of care is progression. We educate patients on progressing their care when they return home. It’s not much good if you can only heal at the clinic, and a solid understanding of how and when to progress is crucial for long-lasting recovery.
For each appointment, we establish new goals by looking at what you could tolerate in the previous appointment. From there, we gradually push the system inch by inch, ensuring the new stimulus is strong enough to continually change the function. It’s no different than increasing the weight in your fitness routine. To adapt, you need new challenges.
Increasing the difficulty of neurologic exercises can come in several forms, which are outlined below.
-More repetitions
-Increasing the speed at which you perform the exercises
-Moving from lying to sitting to standing to standing heel to toe
-Moving from a solid surface to a foam surface to eyes closes
-Performing exercises to a metronome and speeding it up gradually
-Increasing the complexity of the background
-Increasing the light and sound during exercises
These are just a few ways we help teach patients to progress their at-home programs. Our focus is crafting a plan that provides relief in the clinic and continually provides relief for long enough to create plasticity. This is the key to sustaining symptom relief, and we pride ourselves on it.
To see if our intensive program is a good fit, click here to schedule a consultation with one of our doctors. Click here to read our 100+ Google reviews of people who have gone through our intensive programs.
Helpful Tips for Managing Concussion Neck Pain
Neck pain after a concussion is annoying and problematic, to say the least, but it’s not a life sentence. With the proper care and support, it can be quickly resolved. Below are some helpful tips we’ve used with patients to manage symptoms when they flair.
Don’t Bulldoze Symptoms
Many people we work with are highly motivated to improve. They sometimes feel symptoms and push through them anyway, only to pay the price later. Let symptoms be an indicator that you need a break. Allowing your system the time it needs to recover will help you function at a higher level and accelerate your recovery dramatically.
Nutrition
A balanced diet can accelerate recovery in various ways following a concussion. Prioritize foods high in healthy, unsaturated fat and rich in antioxidants. Consider supplementing fish oil, turmeric, and electrolytes to accelerate the natural healing process that occurs within the first few months of recovery.
Move Your Body Safely
Finding a form of physical activity that doesn’t trigger symptoms is a huge part of recovery. It’s intuitive to reduce movement if it makes you worse, but this can lead to deconditioning and create a more significant barrier to entry when you start the recovery process. Try to find any form of activity that works for you. For a best practice for symptom prevention, click here for an overview of the Buffalo Concussion Treadmill Protocol.
Sprint Mentality vs. Marathon Mentality
Many find adopting a more sprint mentality throughout the day helpful. This means dedicating small chunks of time to focus exclusively on getting things done and then allowing the system to recover. Not only will this help you stay on task and improve productivity, but it will also give your brain the rest it needs to recover and avoid a crash.
Avoid Excessive Caffeine, Nicotine, and Alcohol
During concussion recovery, avoid these three things until your symptoms have stabilized. Caffeine and alcohol naturally cause the body to shed water, leading to dehydration and electrolyte imbalances. Nicotine tends to ramp up anxiety, which is usually present in post-concussion headaches.
Find Support
Recovering from a concussion can quickly become isolating. Try not to socially isolate yourself, and reach out to your friends and family for support. The snowball of anxiety and catastrophizing your symptoms does not lead to anywhere good. If you feel this happens, reach out and get your thoughts into the open before they cascade into more symptoms.
De-Stress
Concussion recovery is stressful on its own. Add in life stress, and it can quickly become overwhelming. Try guided mindfulness meditation, yoga, therapy, or vagal nerve stimulation. These techniques and therapies can help reduce the body’s stress response and ease the emotional pain associated with a prolonged recovery.
If you have questions about concussion recovery, click here to schedule a complimentary consultation with one of our doctors. We’ve treated hundreds of complex neurologic cases and can help piece together the missing pieces in your recovery.
*Note: The information provided in this article is for educational purposes only and does not constitute a doctor-patient relationship. Patients should consult their medical provider or primary care physician before trying any remedies or therapies at home.

