Post Concussion Headaches
Headaches are the most common symptom following a concussion. An overwhelming majority of people will experience some form of post-concussion headache in their recovery, often lasting days to weeks. There is a subset of people who will transition to chronic headaches after a concussion, which will last for months to years following the injury. Chronic headaches come with their own unique set of challenges, often occurring with other concussion symptoms like dizziness, brain fog, anxiety/depression, and eye strain.
While post-concussion headaches can come in many forms, the most common are tension-type headaches and migraine headaches. Tension headaches are commonly described as a vice around your forehead and tend to worsen with high stress. Migraine attacks are more nuanced and are commonly misdiagnosed due to vague diagnostic criteria. We mention these two because it is common for both of them to be resistant to medication. If you’ve been medicated for concussion headaches with little to no success, you’re not alone.
Furthermore, many of the medications can worsen concussion headaches or cause something called a “rebound headache.” For example, some of the side effects listed on several medications commonly prescribed for headaches are, in fact, headaches. Rebound headaches are a staple in migraine sufferers and result from the body not being able to detox the meds fast enough.
The point is, if you’re stuck in a perpetual state of headache that is resistant to medications, you’ll likely need a multidisciplinary form of treatment that addresses all aspects of what’s driving your headaches. This may mean multiple types of providers at once or a facility that has a well-rounded approach that borrows concepts from different branches of medicine. Either way, searching for the right combination can be challenging, frustrating, and expensive. This article will help you cut to the chase and find the care you need faster and more effectively.
In this article, we’ll look at:
-What are post-concussion headaches
-Types of post-concussion headaches
-Causes of post-concussion headaches
-Treatment options for post-concussion headaches
-Helpful tips
If you’re reading this and you or someone you love is struggling with ongoing dizziness symptoms, click here for a free consultation with one of our doctors. The Neural Connection specializes in stubborn post-concussion symptoms. Our doctors will carefully listen to your situation and make the appropriate recommendation, even if it’s not with us. Click here to schedule a consultation, and click here to see our 100+ 5-star reviews from people just like you.
What Are Post-Concussion Headaches?
Headaches and concussions almost always happen together. Of all post-concussion symptoms, headaches are the most common. Up to 90% of people will experience a headache following a concussion/mild traumatic brain injury. Post-concussion headaches are considered a “Secondary disorder,” which means they happen as the result of the concussion. By definition, headaches begin within 7 days of the injury, which can be misleading as some headaches take weeks or even months to show up.
Concussion headaches are generally classified by how long they take to show up and go away. Headaches that present and resolve within 3 months of the injury are considered “acute.” Headaches that last more than 3 months are labeled as chronic and, in our experience, require a much different treatment strategy than acute headaches. In our clinical experience, it is not uncommon for patients to still have headaches 6 months to a year following their concussion. Some common risk factors that predispose you to having chronic concussion headaches are
-Family history of headaches
-Previous chronic headaches
-Being a woman
-Other headache conditions, like migraine or tension-type headaches
-Neck involvement from the initial concussion
-Immediate onset of headache following concussion
-Prior history of concussion
-History of anxiety-related disorder
-Previous chronic pain diagnosis
-Loss of consciousness after concussion
-Presence of sleep-related disorder
If you’re predisposed to migraine attacks before your concussion, they will likely increase in severity. You may also develop an entirely separate type of headache that closely mimics the symptoms of a migraine attack. Similarly, tension-type headaches will typically increase in frequency and intensity.
It’s essential to bring this information to your appointments, as we commonly see a lot of overlap between types of headaches. This leads to misdiagnosis and trying to manage a post-concussion headache like a migraine, which doesn’t work. Now, we’ll dive into the types of concussion headaches and what distinguishes them from other types of headaches.
Types of Post-Concussion Headaches
Concussion headaches can come in many shapes, sizes, and timelines. Many will often feel local pain and tenderness where the injury occurred, while some will feel nothing for weeks and suddenly develop diffuse pain that is hard to pinpoint. The most common places for pain to settle are in the temples, across the forehead, the top of the neck beneath the skull, deep within the eyes, and in the neck.
Keep in mind these aches and pains occur for various reasons. You’re also allowed to have more than one type happening together. This is one reason why diagnosing concussion headaches can be challenging.
One way around this is to develop a plan to document your symptoms and when/where they occur. Keeping this log is not only helpful for you in identifying triggers, but it can also be helpful for your providers. It’s difficult to concisely describe your symptoms within minutes of meeting a new doctor. A detailed log will make it easier for providers to cut through the details and get an accurate diagnosis. Some things to write down are when the pain started, what you were doing, how long it lasted, intensity, and any words to describe it like local, diffuse (all over), sharp, etc.
Some common diagnoses for concussion headaches are:
-Tension headaches
-Migraines
-Cervicogenic headaches
-Cluster Headaches
-Rebound headaches
-TMJ headaches
-Dysautonomia Headaches
Let’s dive into each of these so you can better understand how to manage them.
Concussion Headaches: Tension-Type Headache
Tension-type headaches account for roughly 30% of post-concussion complaints. They can occur immediately following the concussion or result from a combination of other factors we will discuss later. They are classically defined as a feeling of pressure in the head, particularly in or around the forehead. Patients commonly describe it as a vice squeezing their forehead. They often report they get worse in times of stress or when other symptoms are present.
While the cause of a tension headache is often challenging to pin down to one specific thing, the soft tissues usually involved are in the upper cervical spine, just below the base of the skull. The pain pattern often begins here and spreads to the upper back, temples, and sometimes the top of the head.
Below is a list of descriptors patients will often use:
-Pressure or squeezing around the forehead or in any area of the skull
-Symptoms progress as the day goes on
-Mild to moderate intensity with a dull or aching quality
-Coincides with neck pain from accident
-Gets worse with other symptoms or with stress
-Progresses gradually and peaks within the hour, usually lasting between 30 minutes to a few hours
-Light and sound sensitivity during peak symptoms
-Occasionally comes with dizziness and nausea
-Resistant to medications
-Worse with sudden head movements or prolonged poor posture
-Elevated heart rate and blood pressure
Many of the symptoms listed above involve the autonomic nervous system (ANS). This branch of your nervous system controls the balance of fight/ flight and recovery processes. While the ANS can cause a different type of headache, this involvement can worsen tension-type headaches. We’ll go over this later, but this fact illustrates how challenging it can be to attribute the source of a tension headache to one thing. As a generalization, we describe tension headaches as a combination of cervical injury and autonomic dysfunction.

Post Concussion Headaches: Migraine
Migraine attacks are a disabling condition on their own. When you add in concussion symptoms, they can quickly snowball into some of the most painful and problematic post-concussion complications. It should be noted that migraine attacks are a primary condition, and headaches are a side effect of a much larger neurologic condition. They often get lumped in with headaches, which is frustrating and a source of stress for those who suffer from them regularly.
One of the challenges with managing post-concussion migraine attacks is the tendency to misdiagnose them. Actual migraine is a genetic condition that typically starts at the onset of puberty and worsens into the 30s and 40s. It is one of the most commonly misdiagnosed conditions due to the ambiguity of the diagnostic criteria listed below.
- At least five headache episodes fulfilling criteria B-D
- Headache attacks lasting 4-72 hours (untreated or unsuccessfully treated)
- Headache with at least two of the following characteristics:
- Unilateral location
- Pulsating quality
- Moderate or severe pain intensity
- Aggravation by or causing avoidance of routine physical activity
- During a headache, at least one of the following:
- Nausea and/or vomiting
- Photophobia and phonophobia
Many headache disorders fit this criteria, leading to the overdiagnosis of migraine. Specific to concussion, it’s easy to see why many post-concussion headaches get misdiagnosed as migraine. As previously mentioned, headaches that aren’t migraines do not typically respond to medication. If you’re having the same symptoms listed above, but the medication isn’t working, you likely have a combination of other headaches.
However, it’s not uncommon for people previously diagnosed with migraine to sustain a concussion and suddenly experience a rapid increase in attack frequency and intensity. If this is the case, you’ll likely benefit more from addressing the underlying reason for the rise in attacks and not simply modifying medication.
Within the migraine diagnosis comes a plethora of other subdiagnoses. For example, vestibular migraine, ocular migraine, abdominal migraine, migraine with aura, and silent migraine are all technically different versions of the same condition.
To simplify this, we use the following analogy. Every person has a bucket, and when the bucket overflows, you get a migraine. The bucket represents your autonomic nervous system and its capacity to metabolize stress. You either have a bucket problem or a faucet problem. The faucets represent stressors that metaphorically drip water into the bucket. These come in the form of hormones, food, concussion symptoms, cervical spine dysfunction, gut dysfunction, and low-level infections. Diagnosing which type of migraine you have comes down to figuring out if it’s a bucket problem or a faucet problem.
Another way of thinking about it is by examining the migraine process. When a migraine begins, a seizure-like activity pattern sweeps through the brain, starting in the back. The occipital cortex, which processes vision, is usually where symptoms start, which explains why some get a visual symptom called a scotoma at the onset of a migraine. As this process, known as a “cortical spreading depression,” sweeps through the brain, any area that is weak or unstable cannot sustain its regular activity, metabolically fails, and produces symptoms. In this sense, most migraine attacks are the same, but different areas fail and produce symptoms.
The bottom line is this: if you sustained a concussion and you never had a migraine attack in your life until the injury, you probably don’t have actual migraines. If you had them before the accident and now they’re worse, your post-concussion symptoms are the main trigger for your attacks, and you’ll benefit from addressing the underlying concussive damage.
Further Reading: Managing Chronic Headaches

Post Concussion Headaches: Cervicogenic Headaches
Cervicogenic means a headache coming from the neck. This can involve the neck’s soft tissues, bones, ligaments, or tendons. These are especially common after a whiplash injury, disrupting the structure and feedback from the neck bones and muscles. As a general rule, following a concussion, you’ll want to rule out any hard structural damage through imaging modalities like an MRI, X-ray, or CT scan. Assuming nothing is broken, you’ll want to identify which structures were affected and seek treatment to restore normal function.
Some common symptoms of cervicogenic headaches are listed below.
-Headaches that start at the top of the neck, just below the base of the skull.
-Coat hanger distribution of pain, which is classically defined as pain that starts in the upper back and travels up into the base of the skull
-Mild to severe pain described as dull, achy, persistent, and occasionally radiating
-Dizziness and nausea with a lot of movement
-Stiffness and loss of range of motion
-Worse in busy visual environments (if visual-vestibular symptoms are also present)
-Relieved by musculoskeletal therapies like massage, chiropractic, and acupuncture.
Cervicogenic headaches can be straightforward if the only complication is damage to the neck structures. As we’ll cover later, however, people often face challenges when neck damage is combined with vestibular damage or problems with how their eyes track.

Post Concussion Headaches: Cluster Headaches
It’s rare for a concussion to induce cluster headache attacks on its own. However, if you were previously susceptible to them and then sustained a concussion, it can ramp up the frequency and intensity. Cluster headaches are described as sharp, sudden, intense stabbing pain behind one eye, lasting minutes to hours. They usually resolve as quickly as they come on. Medical treatments typically come in the form of injections, nerve blocks, and medications. Conservative treatments often involve vagal nerve stimulation and supplemental oxygen.
Common symptoms of cluster headaches include:
-Sudden, sharp pain behind one eye
-Tearing and redness of the affected eye
-Sinus congestion
-Ptosis (droopy eyelid) on the affected side
-Light and sound sensitivity
-Nausea
-Post-attack headache
Post Concussion Headaches: Medication Overuse and Rebound Headaches
Over-the-counter painkillers and prescription medication are often a first line of treatment for those suffering from post-concussion headaches. If you’re one of the lucky ones who don’t get lingering headaches, this is usually not an issue. Problems arise when you take these too long; they create a secondary type of headache called a rebound headache. These are sometimes referred to as medication overuse headaches, which apply more to prescription migraine medication.
These headaches affect roughly 40% of people taking painkillers for post-concussion headaches. The good news is once you stop taking these medications, the rebound headaches usually subside. It can get a little trickier when you’re dealing with prescription medication, so if this is the case, please get in touch with your prescribing physician to discuss the process of tapering off.
These can be challenging because the symptoms from overusing the medication can often closely resemble the symptoms you’re taking them for. Some common traits of rebound headaches include:
-Began after beginning the use of medication
-Improved by the cessation of medication
-Dull, throbbing, or pounding pain
-Diffuse pain in the front, back, or top of the head
-Nausea
-Irritability
-A “hangover” like sensation, especially in the morning
Causes of Concussion Headaches
Even though headaches after a concussion are very common, diagnosing the source can be somewhat of a shell game. Several sources often compete with one another, sometimes requiring multiple forms of treatment. Some of the common sources we see in the clinic are listed below.
-Autonomic issues
-Vestibular System
-Vision and eye-tracking issues
-Mismatches between sensory systems
-Sleep problems
-Unresolved whiplash
-Psychological symptoms
Further Reading: Post Traumatic Headache
Autonomic Nervous System (ANS) Dysfunction
One of the most common underlying sources of headache after a concussion is dysregulation of the autonomic nervous system. This nervous system branch is easily understood as the balance between “fight or flight” and “rest and digest” responses. This see-saw-like relationship helps your body prepare itself to deal with stress or winds you down so you can recover.
The main functions of the ANS include heart rate, blood pressure, breathing rate, and glucose metabolism. Imagine you just got the worst news of your life and need to run home ASAP. Your breathing is faster, your heart rate and blood pressure go up, your pupils dilate to let in more light, and your body pulls sugar out of storage so you have quick energy to burn. This same process can happen to a lesser degree after a concussion, especially when your equilibrium is off.
Patients with prolonged autonomic dysfunction often report feelings of head pressure, tightness in the chest, and, over time, an overwhelming sense of fatigue. An easy way to test whether or not your concussion has autonomic components is to perform something called the Buffalo Concussion Treadmill Test. It’s essentially light cardio with the aim of producing symptoms. If you perform this test and your symptoms get worse after exertion, you probably have some degree of autonomic involvement with your concussion.
Autonomic dysfunction is especially common in migraine and tension-type headaches. It is also nearly universal in concussions that have a combined presentation, meaning symptoms stemming from multiple sources. More on that later.
Further Reading: POTS After a Concussion

Vestibular Issues
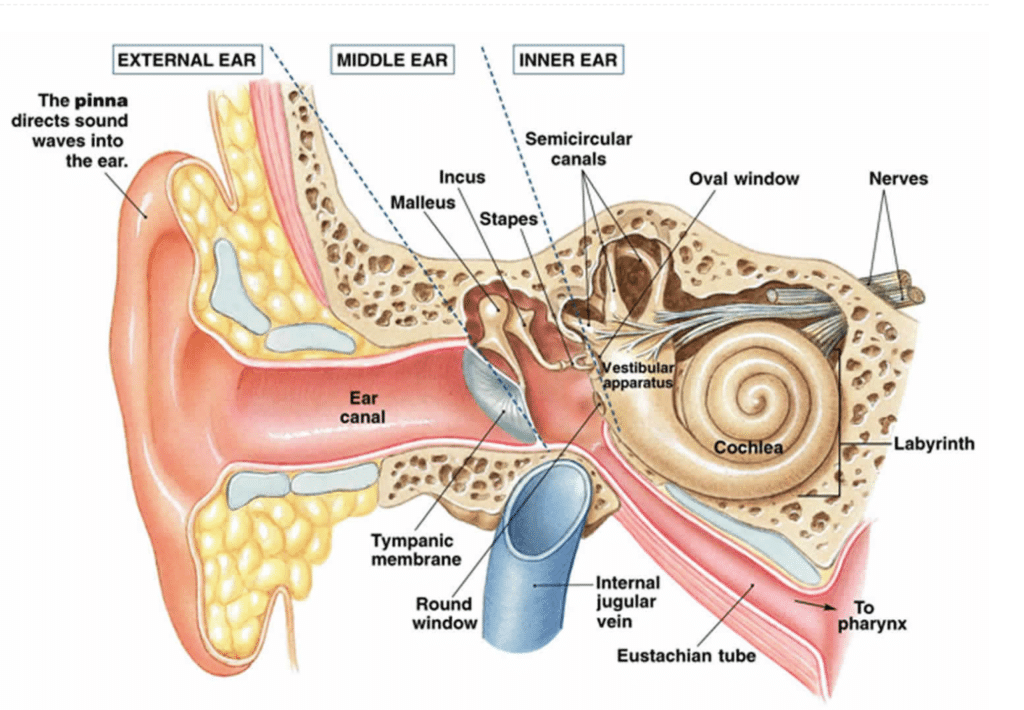
The vestibular system does much more than keep you from falling over. This intricate system of parts is located in your temporal bone, commonly referred to as the “inner ear.” Its primary job is to sense how and how much the body and head are moving. It then combines that information with other senses (eyes and muscles in the neck) to let your brain know what’s happening.
Aside from these vital functions, it also controls blood flow into the head. We perform a modified tilt table test, assessing the vestibular system’s ability to push blood into the head when rising from on your back to fully upright. With this in mind, it’s easy to see why vestibular dysfunction often leads to autonomic headaches.
Furthermore, issues arise when a concussion disrupts the input from the vestibular organ. This results in a mismatch between systems, leading to an intense dizziness and stress response. It’s similar to being very motion-sick in a car, but all of the time. Once the brain flags the vestibular input as wrong, it typically relies more on the other two senses (vision and muscles in the neck) for the same information. This leads to more tension in the neck (leading to headaches that don’t respond to muscle-based therapies) or an overreliance on vision for input on movement. An over-reliance on visual input leaves people susceptible to challenges in areas with a lot of movement, such as grocery stores, sporting events, or malls.
Some common symptoms associated with vestibular dysfunction are:
-Nausea
-Lightheadedness, especially after exertion
-Pain on the side of vestibular damage
-Headaches that don’t respond to musculoskeletal care
-Problems being in busy visual environments
-Motion sickness
-Feeling unsteady on your feet
-Light and sound sensitivity
-Tinnitus (ringing in ears)
-Pulsing headaches
-Anxiety
Further Reading: Picking the Right Inner Ear Test
Vision and Eye Tracking Problems
Concussions often affect the eyes, both in terms of how they see and how they move. Damage often occurs to the area in the back of the brain that processes vision and to areas in the brainstem that control how the eyes move. People with damage to these visual processing areas will often struggle greatly with prolonged screen time, reading, focusing for extended periods of time, and being in busy visual environments.
In our clinic, we assess for components of binocular vision dysfunction, commonly referred to as BVD. We look at how well the eyes can hold on to a target, how smoothly they follow things in their environment, how well they jump from one thing to another, alignment in the skull, optokinetic reflexes, and several others.
We check for errors in these functions, and more errors mean more symptoms.
Common symptoms associated with visual dysfunction are:
-Tension-type headaches around the eyes
-Light sensitivity
-Fatigue and headache with prolonged screen time or reading
-Dizziness
-Double vision when fatigued
-Disorientation when looking at something close, then suddenly looking at something far away
-Nausea and discomfort when looking at something too close
-Nausea and headaches in busy visual environments
-New head tilt or rotation at rest
Mismatches Between Sensory Systems
This is one of our clinic’s most challenging and standard presentations. Concussions rarely affect one system in isolation, and the combination of visual, vestibular, and cervical issues is challenging for any provider to encounter. The problem lies in the way healthcare is siloed. It’s often helpful to have people who are very specialized in their niche, but this is one instance where it’s an obstacle.
For example, eye-tracking issues are commonly seen first by a neuro-optometrist. A vestibular physical therapist often handles dizziness. Neck problems and headaches are commonly treated by chiropractors, massage therapists, or acupuncturists. The list goes on. Getting a cohesive program that integrates all these systems is challenging when you have 3-6 doctors with different licenses working on the same case. There are no guarantees that they all speak and will listen to each other in the name of a comprehensive plan for your unique needs.
As mentioned in previous sections, disagreeing with these systems has consequences. These typically include dizziness, stress, headaches, nausea, time, and money. The best approach to treating these issues is to find a provider trained to integrate them. The paradigm is commonly referred to as “central vestibular rehab,” as opposed to the peripheral model most of the medical field operates in. Central vestibular rehab focuses on getting all these systems to learn to speak the same language.
If you’re reading this and this sounds like your main issue, click here for a free consultation with one of our doctors. The Neural Connection specializes in stubborn post-concussion symptoms and central vestibular rehabilitation. Our doctors will carefully listen to your situation and make the appropriate recommendation, even if it’s not with us. Click here to schedule a consultation, and click here to see our 100+ 5-star reviews from people just like you.
Sleep Problems and Poor Recovery
Sleep problems after a concussion can seem paradoxical. You feel stressed out and wired most of the day, wishing you had time to nap and take a moment. Then, bedtime comes, and you feel more awake than ever. The issue lives in something called the HPA axis. The H in this, named after the hypothalamus, can become disrupted due to prolonged periods of elevated stress.
The HPA axis is largely responsible for producing stress hormones, among other things. Dysfunction in the system or outright injury to the deep structures in the brain can lead to problems creating the hormones necessary to fall asleep. This makes recovery more difficult, leading to a snowball of symptoms.
Further reading: Insert article about sleep
Untreated Whiplash
The seven most common symptoms of whiplash and the seven most common symptoms of concussion are nearly identical.

Not only do both symptoms overlap, but the treatment is also consistent. Whiplash headaches often present as upper back tightness that wraps up into the base of the skull, into the temples, occasionally to the top of the head, and into the eyes.
The mechanism of whiplash is different from that of other forms of injury. It is classified as a rapid acceleration and deceleration of the head, which strains and occasionally tears the muscles and ligaments in the cervical spine. Given the nature of this injury, it makes sense that concussions also occur, given the brain’s tendency to bounce around in the skull.
In our experience, treating other concussion issues while you rehab the soft tissues in the neck gives you the best chance for a full recovery. Additionally, one aspect of whiplash rehab that goes under-treated is the feedback coming from the neck soft tissues.
The current healthcare landscape does well with mobility, strength, and alignment, but few comprehensively address the feedback. What this means is how accurate the signals coming from the neck are. When they are inaccurate, the mismatch we discussed earlier causes all the resultant nausea and motion sickness.
We use a lot of visual feedback in our office to treat this. We have special glasses that allow you to see the feedback from the neck and visualize where and how much it breaks down. This feedback is valuable for rehab because it will enable you to re-teach your brain what good feedback looks like and accelerate the healing process.
Further reading: Untreated whiplash symptoms & treatment
Psychological Difficulties
Mood disorders are commonly a side effect of concussions. Depression and anxiety are 2 of the more common complications following an injury. Around half of patients will experience one or both in the first year of recovery. These can stem from outright damage to the limbic areas of the brain or due to the long and challenging recoveries some people face.
Furthermore, if you’re already susceptible to anxiety, the influx of stress hormones stemming from the injury can often combine with pre-existing anxiety and make it worse. Seeking out professional counseling, finding support groups, stress reduction techniques like meditation and yoga, and therapeutic techniques like EMDR are all helpful resources in the healing process.
If you’re dealing with ongoing mental health struggles following a concussion, know you’re not alone, and it’s a common symptom in recovery. It can be scary and challenging to not know whether or not you’ll make a full recovery, and it’s ok to have those emotions. Just know they’re temporary and ok to have, and this too shall pass.
Treating Concussion Headaches
I’m sure by now you realize what a challenge effectively treating concussion headaches can be. There are many combinations of causes and an ever-greater number of specialists who may or may not be able to help. This section will review all the options and help you decide what options are best for you.
A Note on Medications.
A concussion will often land you in a doctor’s office, making sure nothing is outright broken in your head. While this is a good first point of contact and the right decision for your safety, understand that the job of a medical provider is not necessarily to improve your quality of life. Their job is to preserve your life.
This is an important distinction because many people will say, “Nothing is broken, so you should be fine.” This can be confusing and emotionally hard to swallow when you know something is off. They’re looking for things that can be treated with medications, surgery, or injections most of the time. On that note, there are currently no FDA-approved medications to treat concussions. Furthermore, many headaches, even if they’re not truly migraine, will get medicated with drugs that have many well-documented side effects, many of which you may be struggling to find relief for.
For example, many people will get prescribed the medication sumatriptan for a post-concussion headache that looks like a migraine. Some of the listed side effects of this medication are “headache, dizziness, nausea, and confusion.” The point is, be weary of relying on medication to resolve your post-concussion issues. They are typically unaffected by post-concussion symptoms, and if you’re not dealing with genuine, genetic migraine, they will likely make your other concussion symptoms worse.
Treating Concussion Headaches Holistically
We’ve seen hundreds, if not thousands, of post-concussion cases in our career at The Neural Connection.
Our process starts with a consultation to ensure it’s the right time for this type of treatment. This involves a 30-minute phone call during which one of our doctors will discuss your medical history, what’s worked, what hasn’t, etc. This is important because it allows us to either make the most appropriate referral to something that will help right now or recommend proceeding with an examination.
If the person is a good candidate, they will come in for our initial examination. It starts with a history based on the information provided in the intake. We’ll also review some questionnaire forms to understand emotional status, readiness for change, cognitive function, etc.
Once we grasp the situation well, we jump into our comprehensive battery of tests. We start with a VNG, which allows us to diagnose exactly where the vestibular system is damaged and to what extent. It also allows us to quantify ocular tracking, the ability to follow objects and several other aspects of the visual system.
We then move to autonomic testing to see whether or not the ANS is causing any of the symptoms. From there, we test the injury’s neck and other orthopedic aspects to see how much physical rehabilitation needs to be integrated into the program. Finally, we perform an entire bedside exam to develop an understanding of any other small detail that might help us pick the right therapies.
From there, if the person is a good candidate for care, we’ll recommend several options. With every option, the goal is to achieve “plasticity.” This is the process of physically re-wiring new pathways into the brain with repetition and gradual increases in intensity. It’s the same process that happens when you’re learning something new. At first, you need a lot of repetition to keep the information, but eventually, you have it so memorized that you no longer need to read it. That’s plasticity at work. Forming new habits works the same way.
To achieve plasticity, patients often elect to use our intensive model. Out-of-town patients come for a week and make three appointments a day. They are then given an at-home therapy program to finish cementing the plasticity process. The intense nature of the program jump-starts the process of creating the proteins necessary for plasticity. Then, with enough repetition and intensity at home, the system requires a new pathway. This allows our therapy to continually provide lasting relief into the future.
Local patients typically elect for a slower process known as the 21-day intensive. It’s the same number of appointments, just spread out over 3 weeks instead of 1. Our 100+ 5-star reviews are primarily from people who did intensive programs, which you can read here.
Steps to an Intensive Program
Each appointment in an intensive will generally follow the same series of events listed below.
Preparation
Patients will warm up for 5-10 minutes on our stationary bike. This helps provide the brain with oxygen and prepares the autonomic system for work. It also helps produce vital chemicals that allow plasticity to occur. We then begin with low-level laser therapy and normatec compression boots. Laser therapy helps create more energy in the tissue we need to work, and the boots help return blood to circulation. We’ll conclude this initial process with some vagal nerve stimulation to ensure the entire system has enough room for rehab.
We’ll typically address underlying autonomic rehab before beginning the second rehab phase, which involves individual system work.

Individual System Rehab
Once the system is prepared for rehab, the first step is vestibular rehab. Think of the vestibular system as the axle of a car. You can’t drive it very fast if the car constantly pulls to one side. Once the system has been integrated, we can move to specific ocular and neck rehab forms. This often comes in the form of eye-tracking exercises, gaze stability work, saccades, and laser-guided cervical proprioception training, just to name a few.
Once these individual systems have had a chance to improve, we move into the 3rd phase of care: Integration exercises.

Integration Exercises.
This is where the rehab begins to stick. Once each system has had a chance to improve, we move into exercises that work all systems simultaneously. Think of it like members of an orchestra. The music won’t sound perfect if the entire band only practices their parts individually. The group needs time to play together to sound good. This is where our program earns its keep. Integrating everything into exercises that work simultaneously allows the system to recalibrate and work as a whole unit. With the siloed nature of concussion care, this aspect is crucial for long-lasting results. Once we get someone here, the focus shifts to progression.
Progression
The final aspect of care is progression. We educate patients on progressing their care when they return home. It’s not much good if you can only heal at the clinic, and a solid understanding of how and when to progress is crucial for long-lasting recovery.
Each appointment we establish new goals by looking at what you could tolerate in the previous appointment. From there, we gradually push the system inch by inch, ensuring the new stimulus is strong enough to continually change the function. It’s no different than increasing the weight in your fitness routine. To adapt, you need new challenges.
Increasing the difficulty of neurologic exercises can come in several forms, which are outlined below.
-More repetitions
-Increasing the speed at which you perform the exercises
-Moving from lying to sitting to standing to standing heel to toe
-Moving from a solid surface to a foam surface to eyes closes
-Performing exercises to a metronome and speeding it up gradually
-Increasing the complexity of the background
-Increasing the light and sound during exercises
These are just a few ways we help teach patients to progress their at-home programs. Our focus is crafting a plan that provides relief in the clinic and continually provides relief for long enough to create plasticity. This is the key to sustaining symptom relief and something we pride ourselves on.
To see if our intensive program is a good fit, click here to schedule a consultation with one of our doctors. Click here to read our 100+ Google reviews of people who have gone through our intensive programs.
Helpful Tips for Managing Concussion Headaches
Post-concussion headaches are annoying and problematic, to say the least, but it’s not a life sentence. With the proper care and support, it can be quickly resolved. Below are some helpful tips we’ve used with patients to manage symptoms when they flair.
Don’t Bulldoze Symptoms
Many people we work with are highly motivated to improve. They sometimes feel symptoms and push through them anyway, only to pay the price later. Let symptoms be an indicator that you need a break. Allowing your system the time it needs to recover will help you function at a higher level and accelerate your recovery dramatically.
Nutrition
A balanced diet can accelerate recovery in various ways following a concussion. Prioritize foods that are high in healthy, unsaturated fat and rich in antioxidants. Consider supplementing fish oil, turmeric, and electrolytes to accelerate the natural healing process that occurs within the first few months of recovery.
Move Your Body Safely
Finding a form of physical activity that doesn’t trigger symptoms is a huge part of recovery. It’s intuitive to reduce movement if it makes you worse, but this can lead to deconditioning and create a more significant barrier to entry when you start the recovery process. Try and find any form of activity that works for you. For a best practice for symptom prevention, click here for an overview of the Buffalo Concussion Treadmill Protocol.
Sprint Mentality vs. Marathon Mentality
Many find adopting more of a sprint mentality throughout the day helpful. This means dedicating small chunks of time to focus exclusively on getting things done and then allowing the system to recover. Not only will this help you stay on task and improve productivity, but it will also give your brain the rest it needs to recover and avoid a crash.
Avoid Excessive Caffeine, Nicotine, and Alcohol
During concussion recovery, avoid these 3 things until your symptoms have stabilized. Caffeine and alcohol naturally cause the body to shed water, leading to dehydration and electrolyte imbalances. Nicotine tends to ramp up anxiety, which is usually present in post-concussion headaches.
Find Support
Recovering from a concussion can quickly become isolating. Try not to socially isolate yourself, and reach out to your friends and family for support. The snowball of anxiety and catastrophizing your symptoms does not lead to anywhere good. If you feel this happens, reach out and get your thoughts into the open before they cascade into more symptoms.
De-Stress
Concussion recovery is stressful on its own. Add in life stress, and it can quickly become overwhelming. Try guided mindfulness meditation, yoga, therapy, or vagal nerve stimulation. These techniques and therapies can help reduce the body’s stress response and ease the emotional pain associated with a prolonged recovery.
Other Helpful Therapies for Concussion Headaches
In our decades of experience, we’ve heard of almost everything people have tried. Some have been successful, and we’ve provided a list below of things we’ve heard have been beneficial at some point in the recovery.
- Cognitive Rehabilitation Therapy: CBT helps you recognize thought patterns and environmental factors that perpetuate unhelpful thought patterns. It might help overcome thoughts like “I’m never going to get better” or assist in preventing a thought from snowballing into unhelpful, depressing thought patterns.
- Yoga Nidra: This form of meditation is especially helpful for tension headaches and migraine attacks. It focuses on physical relaxation by scanning body regions for tension and using breathing techniques to relax overactive muscle groups.
- Acupuncture: Some people prefer acupuncture because it can be less intense and jarring than a chiropractic adjustment or a deep tissue massage. There is promising research on its benefits for different types of headaches and concussion symptoms.
- Intermittent Fasting: Fasting is a great way to increase a process known as “autophagy.” This is the process of “taking out the garbage” and removing dead or injured cells. Be cautious if you have pre-existing blood sugar regulation issues.
- Dietary Changes: Many benefit from a gluten and dairy-free lifestyle in the beginning and intermediate stages of concussion recovery. A diet that prioritizes blood sugar regulation can add stability to the system and reduce some aspects of autonomic headaches.
If you have questions about concussion recovery, click here to schedule a complimentary consultation with one of our doctors. We’ve treated hundreds of complex neurologic cases and can help piece together the missing pieces in your recovery.
*Note: The information provided in this article is for educational purposes only and does not constitute a doctor-patient relationship. Patients should consult their medical provider or primary care physician before trying any remedies or therapies at home.

