Balance Problems & Dizziness After a Concussion: Causes and Treatments
Feeling off balance following a brain injury is a widespread complaint, with upward of 50% of patients reporting some balance difficulty during their recovery. People usually recover in days to weeks, but it is not uncommon for people to struggle with ongoing dizziness for months to years after the initial injury. On top of that, dizziness rarely occurs in isolation. Symptoms like headaches, nausea, cognitive challenges, and mood issues often accompany feeling off balance.
Vestibular rehabilitation is a staple of the recovery process. Its goal is to rebalance the intricate vestibular system so there is no longer a false sense of movement. The problem lies in the complex nature of concussions. Vestibular therapy is often enough to recalibrate the vestibular system, but if dizziness exists with other issues stemming from the concussion, things can get complex.
This article will serve as a resource to help you navigate the world of vestibular care. We’ll cover common symptoms, causes, diagnostic procedures, and different types of vestibular therapy. It will save you time, energy, and money finding the right combination of treatments and cut through a lot of the learning curve that comes with prolonged concussion symptoms. Let’s dive in.
Table of Contents:
-
- Symptoms
-
- Causes
-
- Diagnosis
-
- Vestibular therapy
-
- Comprehensive post-concussion treatment
-
- Tips to cope with concussion-related balance issues
If you’re reading this and you or someone you love is struggling with ongoing dizziness symptoms, click here for a free consultation with one of our doctors. The Neural Connection specializes in stubborn post-concussion symptoms. Our doctors will carefully listen to your situation and make the appropriate recommendation, even if it’s not with us. Click here to schedule a consultation, and click here to see our 100+ 5-star reviews from people just like you.
Feeling Off Balance is a Common Symptom After a Concussion
The statistics show that around half of patients will suffer from post-concussion. This can take various forms. For example, people often describe a sensation that they’re spinning, the room is spinning, they’re on a boat, or they feel “off balance and nauseous.” This information helps diagnose precisely where the dizziness is coming from and what treatment will effectively manage symptoms.
Other symptoms that commonly occur with dizziness are:
-Feeling lightheaded
-Fainting
-Feeling like you need to sit down when you stand up too fast
-A sensation of bobbing up and down and floating in the water
-Disorientation
-Not trusting your feet or a general feeling of unsteadiness
-Tripping while walking
-Elevated heart rate
-Unexplained anxiety or panic attacks
-Heaviness in your head
-Trouble walking in a straight line
-A sensation of being disconnected from your body
-Excessive postural sway at rest
-Feeling like you’re going to fall over with your eyes closed
-Nausea with your eyes closed
-Suddenly waking up after turning over in bed
It is common for many of these symptoms to intensify in the first 2 weeks following an injury. Some feel intense dizziness and nausea immediately, while some gradually feel dizzy for weeks to months following the injury. In general, the most injured area will create symptoms first. It often takes the brain a few days or weeks to reach a new equilibrium, which explains why the symptoms can take a while to set in.
For instance, headaches are a common complaint following a concussion, especially with whiplash injuries. Once the headaches subside, commonly the most prominent symptoms, people will notice dizziness as the new most prominent symptom.
It’s important to note when the dizziness occurs. For example, the treatment for dizziness that wakes you up turning over in bed is typically different from that at the grocery store. As we’ll cover later, dizziness comes in several forms, each requiring a different strategy.
Why Am I Dizzy After a Concussion?
As mentioned, post-concussion dizziness can have several causes. The key to achieving fast relief is to identify precisely where the issue is and choose the appropriate treatment promptly. Below are some common root causes of post-concussion dizziness.
Physical Damage to the Vestibular System
Direct impact on the head can often cause structural damage to the organ that sends vestibular signals into the brain. The organ is located in the skull’s temporal bone and is susceptible to injuries that rapidly accelerate and decelerate the head. While the organ can sustain damage, the term “vestibular system” indicates there is more to it than just the organ. It includes areas in the middle of the brainstem called the pons and the cerebellum, which is located behind the brain.
Damage to any part listed above can lead to an asymmetry in vestibular signaling, leading to feeling off balance. For example, damage to the organ can lead to one side not communicating effectively, leading to an asymmetry in input from both sides. Damage to the brain stem can lead to abnormalities in cerebral blood flow, leading to lightheadedness. Lastly, damage to the cerebellum prevents the brain from correcting errors from the organ, leading to stubborn dizziness that doesn’t respond to traditional vestibular therapy.
Because the vestibular organ is part of a larger system, it’s essential to be as specific as possible when sharing details with your healthcare provider. These small details will help them pinpoint the issue accurately.
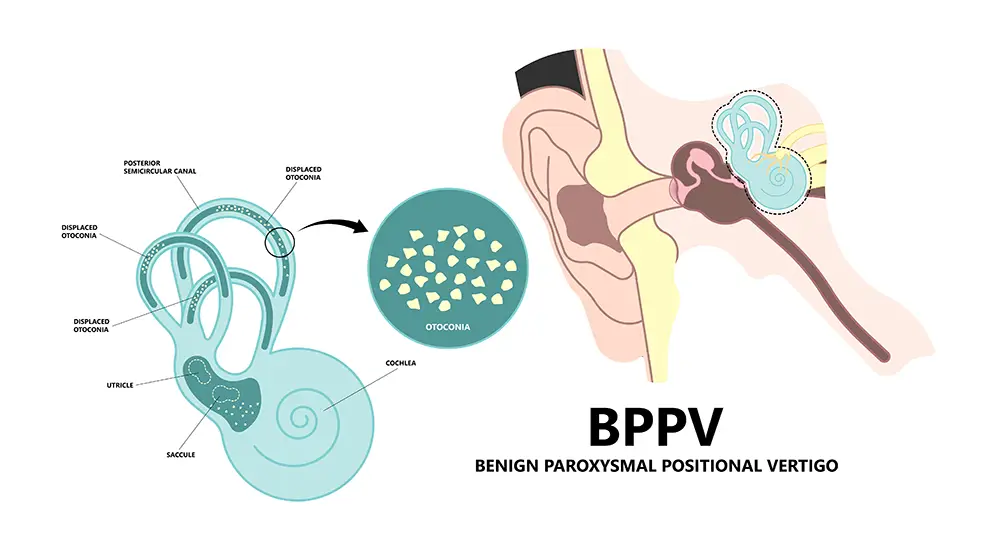
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is one of the most common and easy-to-treat aspects of dizziness. It affects more than half of post-concussion patients and is typically the first thing checked in a dizzy clinic.
BPPV occurs when tiny calcium crystals are shaken and stuck in the vestibular organ. The vestibular system processes more than just rotation. It also processes translation, meaning forward, backward, up, down, and side-to-side. The part of the system that processes these movements is called the “otolithic system.” This system relies on tiny calcium crystals that weigh down a membrane. When you move, the membrane shifts and sends input into the brain when translational movements occur.
Following head trauma, they commonly dislodge from the membrane and fall into the nearby circular canals. These canals process rotational movements rather than translational ones.
When a stone finds its way to the semicircular canal, it disrupts the normal signaling from the vestibular organ when you move your head and activate that specific canal. This results in a rapid onset of intense dizziness.
Treatment for BPPV often involves something called the Epley maneuver. It’s a repositioning maneuver that helps redirect the crystal back to the original starting point. It has a high success rate, with the caveat being it is incredibly uncomfortable and usually elicits a tremendous amount of dizziness while it is occurring. Expect some intense nausea followed by some minor symptoms and eventually symptom resolution.
Damage to the Cervical Spine
Injuries to the brain commonly affect the neck, especially in whiplash injuries. There is a subset of dizziness called “cervicogenic dizziness,” which means dizziness from the neck. When the neck’s soft tissue or bones have been damaged, they no longer send reliable feedback and cause a “mismatch.” This means the input from the neck disagrees with the input from the eyes and balance systems, resulting in an automatic output of stress and dizziness.
It’s important to rule out any serious issues early on. After the injury, consider fractures, ligament damage, and torn muscles. Assuming nothing is damaged or broken, several providers can treat cervical issues. PT is a good first option, along with chiropractic, massage, and/or acupuncture.
A note of caution: if neck issues occur in tandem with other problems (eyes, vestibular, autonomic, etc.), cervical care can often act like a bandaid. Sometimes, the other issue is why the neck is tight, so be vigilant if neck treatments feel suitable for a short time and then return to baseline. This is a good indicator that some other aspect of the injury may lead to the neck tension.
Problems With Blood Flow and Autonomic Function (Dysautonomia)
Sometimes, dizziness can stem from problems with the autonomic nervous system (ANS). This branch of the nervous system can be understood as the “fight or flight” and the “rest and digest systems.” These systems work to balance functions like heart rate, blood pressure, and respiration.
Problems following a concussion can disrupt the balance between these two branches, often resulting in excessive “fight or flight” responses. When these responses go unchecked for long periods of time, parts of the brain that process balance can’t absorb enough blood and oxygen, resulting in symptoms of dizziness and lightheadedness.
Another way the ANS can affect symptoms is through poor adjustments in blood pressure and blood flow upon standing. Most of us have experienced standing up and immediately feeling like we might pass out. Post-concussion autonomic problems can give you this feeling on a regular basis, as small adjustments in blood pressure and blood pressure fail to occur, resulting in ongoing unsteadiness and lightheadedness.
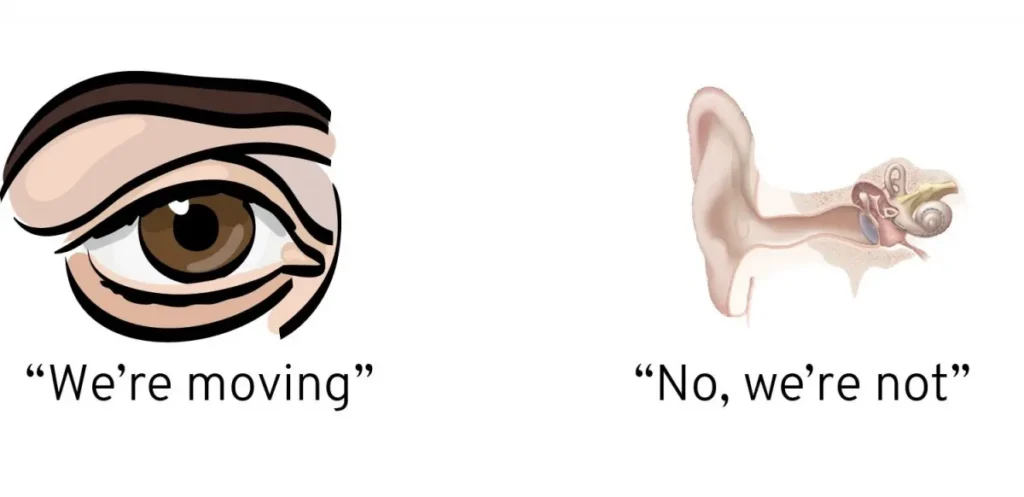
Visual Vestibular Integration
Similar to cervicogenic vertigo, another type of dizziness stems from a mismatch between the eyes and vestibular system. Anytime there is a disagreement between sensory systems, dizziness occurs. This is especially true with the eyes and vestibular system due to their intimate connections.
The connection between the eyes and the vestibular system can easily be seen by looking at something stationary and moving your head side to side or up and down. A reflex called the vestibular-ocular reflex connects the eyes and vestibular system so you can move around the world and keep your eyes fixed on something. Symptoms commonly follow when this reflex breaks down, or the communication between systems is disrupted.
This is one of the issues with traditional concussion care. The providers who treat each issue separately are usually different types of doctors. For example, dizziness is often handled by a physical therapist, while eye issues are commonly treated by an eye doctor. This is where treatment plans can become disjointed, and people will often complain of disjointed care plans with differing opinions.
Familiar environments that bring out visual-vestibular symptoms are
-
- Busy visual environments like shopping malls, grocery stores, or sporting events
-
- Daycare or any setting with a lot of movement in your peripheral vision
-
- Being a passenger in the car and getting motion-sick
-
- Busy paintings or TV motion
-
- Interacting with someone with a lot of movement behind them
-
- Windshield wipers
-
- Lights turning on and off
If this describes your problem, consider contacting one of our providers. We see a lot of visual and vestibular dysfunction, and if you’ve tried traditional therapies with little success, we may be able to help. Click here to schedule a free consultation with one of our doctors. We’ll listen carefully and recommend the most effective path forward, even if it’s not with us.
Neuropathy
Issues with how the feet communicate with the brain can cause problems maintaining a good sense of equilibrium. It’s common for people with conditions like diabetes or other forms of neuropathy to develop balance issues.
The feet and ankle muscles send much information to the vestibular system. Without this information, the brain loses a significant amount of input, which can destabilize the vestibular system. We routinely use input through the feet and ankles to drive more input into the vestibular system to stabilize it and calm symptoms during rehab.
This can take the form of vibration through the feet, exercises on one foot to recruit the ankle stabilizers, and toe exercises to regain motor control and independence.
Medication
If you examine the side effects of many medications, you’ll find dizziness a common side effect. We’ve had patients whose entire collection of dizziness symptoms was attributed to medications they were on for anxiety, migraine, or some other physical ailment. The likelihood of having dizziness as a side effect increases with additional medications.
Another thing to look out for with medications is nutrient depletion. It is common for drugs to deplete essential nutrients and minerals like calcium, b vitamins, and magnesium. Since the vestibular system requires specific electrolyte balance to function, check for these depletions carefully.
Psychological Problems
Dizziness and anxiety tend to go hand in hand. We often hear people who have never experienced anxiety will suddenly develop intense anxiety, even when they’re not actively symptomatic. This anxiety, in turn, exacerbates dizziness, and you get a feedback loop that can spiral out of control.
This results from the physiological response to feeling dizzy. The rapid increase in cortisol and adrenaline can mimic the feeling of anxiety. Patients often find it challenging to decipher whether the emotional disturbance is coming from a physical response to dizziness or from emotional reasons.
The term “psychogenic vertigo” is often used to describe emotional symptoms that cause dizziness outright. While this is possible, we usually find that working on both physical and emotional components simultaneously is an effective way to mitigate symptoms and help the person understand where the anxiety is coming from. Sometimes, this understanding and being able to label the source of the anxiety gives the person enough autonomy to mitigate symptoms when they occur effectively.
Diagnosing Post-Concussion Dizziness
Several different professionals can diagnose vestibular issues. Specialists like otologists, neurologists, vestibular PTs, or functional neurology providers. If more serious pathology is suspected, like a ruptured ear drum or a canal dehiscence, seeking a medical provider should be your priority. As a rule of thumb, medical providers like otologists and neurologists can help you rule out things that will require surgery or medication to manage. They will run labs and perform scans like an MRI or a CT to detect physical issues with the organs or metabolic issues that may be directly causing dizziness.
Assuming nothing is broken, you’ll want to consider seeking out tests for vestibular function. This is where vestibular PT and functional neurology come into play. These providers may run lab tests with different reference ranges, balance tests, hearing tests, and visual tests to assess and quantify the function of the vestibular system. The goal is to pinpoint where the dysfunction is and then discuss the available options.

Helpful tip: As a general rule, vestibular dysfunction can be divided into peripheral and central. Peripheral dizziness can be described as issues with the vestibular organ itself. This includes things like BPPV, Meniere’s disease, and fistulas. In general, PT is effective for peripheral dizziness. Central dizziness is a mismatch between different sensory systems or an issue with the cerebellar systems that correct errors in sensory processing. These problems are generally handled more effectively by someone practicing functional neurology. They’re trained to integrate sensory systems and improve cerebellar function.
Vestibular Rehabilitation and Post-Concussion Recovery
Vestibular rehabilitation (VRT) is the most common and effective way to reduce post-concussion dizziness. VRT is designed to correct asymmetries within the vestibular system and help the other senses (eyes and neck) communicate more cohesively.
We use an assessment process called video nystagmography, which uses infrared cameras to assess vestibular and eye tracking. This allows us to quickly and easily pinpoint where the dysfunction is and also track how effective the treatment is. Once we have this information, we can begin gently stimulating the weak areas and measure how intense the treatment needs to be to observe changes.
Some of the different exercises we use in the clinic are listed below.
VOR Exercises (Gaze Stability): These exercises involve moving the head and keeping the eyes fixed on a target. This helps recalibrate the connection between the vestibular organ and the eyes (hence the name “vestibular-ocular reflex). We can take it further and only work the deficient sides until the system is symmetrical.
-Cervical Rehab: The neck is often involved in post-concussion dizziness, and our rehab addresses many of the familiar sources following an injury. Strength and mobility are good places to start, eventually moving into coordination and retraining the feedback. We do so with visual feedback in the form of laser-guided glasses. This feedback lets us pinpoint which range of motion sends incorrect feedback. This information allows us to be very specific about where the rehab needs to be, and it is easy to see progress due to the visual feedback.
Balance training: Since balance involves multiple systems, we can assess which system is lagging and retrain that in the early stages of care. This is done by assessing balance in various settings, such as open and closed eyes, on an unstable surface, etc. This also gives us valuable information about what else needs to be addressed.
-Gait Training: It is common for the natural gait patterns to become disrupted following a concussion. This can affect how people move and walk. Retraining the gait patterns and practicing walking in busy environments is a great way to restore basic function and reduce symptoms from walking around.
-Vagal System: The vagal system creates the “rest and digest” signals in the body. We regularly use different forms of vagal nerve stimulation to improve the brain’s recovery capacity. This includes meditation, breathing exercises, and vagal nerve stimulation. Being dizzy for years can build up a strong stress response, and the opposite branch of the system can’t keep up. This improved recovery often helps people recover between appointments and has a strong ability to reduce anxiety and stress.

Other Treatments for Vestibular Problems
Some patients may need specific treatment for their conditions, such as the Epley maneuver to address BBPV or medications to help patients cope with their symptoms.
Medication
Severe balance issues are often treated with medication. These are typically used in the beginning stages of dizziness and to control extreme symptoms of motion sickness, nausea, and acute dizziness. Some doctors may prescribe strong sedatives to help cope in the immediate term. Anti-anxiety and anti-depression meds are also commonly used. As mentioned above, be sure to ask about side effects and nutrient depletions.
Concussions Can Cause More Than Just Dizziness
While balance problems are common following a concussion, there are often multiple symptoms occurring together. This can include headaches, eye strain, psychological issues, digestion problems, brain fog, memory issues and more.
This is where the world of concussion care can get confusing and expensive. We love our specialists in American healthcare. When you have 5 or more symptoms following a concussion, you can easily end up with multiple specialists in different branches of medicine giving you different advice. Not only can this get confusing due to conflicting advice, it can get expensive. Even worse, you can end up 6 months with a pile of bills and little to no relief.
We have found the most effective way around this is to simultaneously address as many problems as possible. We use the analogy of a Rubix cube. Traditional concussion care has a specialist for each color of the cube. If you’ve ever done a Rubix cube, you know that sometimes you work on one side and mess up the others. Our concussion program focuses on a little bit of every side, allowing us to solve the entire cube and not just one side. This is done by simultaneously addressing vestibular, ocular, cervical, cognitive, emotional, and autonomic symptoms.
Integrated Concussion Care at The Neural Connection
Our process starts with a consultation to ensure it’s the right time for this type of treatment. This involves a 30-minute phone call during which one of our doctors will discuss your medical history, what’s worked, what hasn’t, etc. This is important because it allows us to either make the most appropriate referral to something that will help right now or recommend proceeding with an examination.
If the person is a good candidate, they will come in for our initial examination. It starts with a history based on the information provided in the intake. We’ll also review some questionaire forms to get a sense of emotional status, readiness for change, cognitive function etc.
Once we get a good grasp of the situation, we jump into our comprehensive battery of tests. We start with a VNG, which allows us to diagnose exactly where in the vestibular system is damage and to what extent. It also allows us to quantify ocular tracking, the ability to follow objects, and several other aspects of the visual system.
We then move to autonomic testing to see whether or not the ANS is causing any of the symptoms. From there, we test the injury’s neck and other orthopedic aspects to see to what extent physical rehabilitation needs to be integrated into the program. Finally, we perform an entire bedside exam to develop an understanding of any other small detail that might help us pick the right therapies.
From there, if the person is a good candidate for care, we’ll recommend several options. With every option, the goal is to achieve “plasticity”. This is the process of physically re-wiring new pathways into the brain with repetition and gradual increases in intensity. It’s the same process that happens when you’re learning something new. At first, you need a lot of repetition to keep the information, but eventually, you have it so memorized you no longer need to read it. That’s plasticity at work. Forming new habits works the same way.
To achieve plasticity, patients often elect to use our intensive model. Out-of-town patients come for a week and make three appointments a day. They are then given an at-home therapy program to finish cementing the plasticity process. The intense nature of the program jump-starts the process of creating the proteins necessary for plasticity. Then, with enough repetition and intensity at home, the system requires the new pathway. This is what allows our therapy to continually provide lasting relief well into the future.
Local patients typically elect for a longer process known as the 21-day intensive. It’s the same number of appointments, just spread out over 3 weeks instead of 1. Our 100+ 5-star reviews are mostly from people who did intensive programs, which you can read here.
Steps to an Intensive Program
Each appointment in an intensive will generally follow the same series of events listed below.
Preparation
Patients will warm up for 5-10 minutes on our stationary bike. This helps provide the brain with oxygen and prepares the autonomic system for work. It also helps produce vital chemicals that allow plasticity to occur. We then begin with low level laser therapy and normatec compression boots. Laser therapy helps produce more energy in the tissue we need to work, and the boots help return blood to circulation. We’ll conclude this initial process with some vagal nerve stimulation to ensure the entire system has enough room for rehab.
We’ll typically address underlying autonomic rehab before beginning the second rehab phase, which involves individual system work.

Individual System Rehab
Once the system is prepared for rehab, we begin with vestibular rehab. Think of the vestibular system as the axle of a car. You can’t drive it very fast if the car constantly pulls to one side. Once the system has been integrated, we can move to specific forms of ocular and neck rehab. This often comes in the form of eye tracking exercises, gaze stability work, saccades, and laser-guided cervical proprioception training, just to name a few.
Once these individual systems have had a chance to improve, we move into the 3rd phase of care: Integration exercises.

Integration Exercises.
This is where the rehab begins to stick. Once each system has had a chance to improve, we move into exercises that work all systems simultaneously. Think of it like members of an orchestra. The music won’t sound very good if the entire band only practices their parts individually. The group needs time to play together to sound good. This is where our program earns its keep. Integrating everything into exercises that work simultaneously allows the system to recalibrate and work as a whole unit. With the siloed nature of concussion care, this aspect is crucial for long-lasting results. Once we get someone here, the focus shifts to progression.
Progression
The final aspect of care is progression. We educate patients on progressing their care when they return home. It’s not much good if you can only heal at the clinic, and a solid understanding of how and when to progress is crucial for long-lasting recovery.
Each appointment we establish new goals by looking at what you could tolerate in the previous appointment. From there, we gradually push the system inch by inch, ensuring the new stimulus is strong enough to continually change the function. It’s no different than increasing the weight in your fitness routine. To adapt, you need new challenges.
Increasing the difficulty of neurologic exercises can come in several forms, which are outlined below.
-More repetitions
-Increasing the speed at which you perform the exercises
-Moving from lying to sitting to standing to standing heel to toe
-Moving from a solid surface to a foam surface to eyes closes
-Performing exercises to a metronome and speeding it up gradually
-Increasing the complexity of the background
-Increasing the light and sound during exercises
These are just a few ways we help teach patients to progress their at-home programs. Our focus is crafting a plan that provides relief in the clinic and continually provides relief for long enough to create plasticity. This is the key to sustaining symptom relief and something we pride ourselves on.
To see if our intensive program is a good fit, click here to schedule a consultation with one of our doctors. Click here to read our 100+ Google reviews of people who have gone through our intensive programs.
Helpful Tips for Managing Dizziness
Post-concussion dizziness is annoying and problematic, to say the least, but it’s not a life sentence. With the right care and support, it can be quickly resolved. Below are some helpful tips we’ve used with patients to manage symptoms when they flair.
Don’t Bulldoze Symptoms: Many people we work with are highly motivated to improve. They sometimes feel symptoms and push through them anyway, only to pay the price later. Let symptoms be an indicator that you need a break. Allowing your system the time it needs to recover will help you function at a higher level and accelerate your recovery dramatically.
Move Your Body Safely: Finding a form of physical activity that doesn’t trigger symptoms is a huge part of recovery. It’s intuitive to reduce movement if it makes you worse, but this can lead to deconditioning and create a larger barrier to entry when you start the recovery process. Try and find any form of activity that works for you.
Home Safety: Early in recovery, it is a good practice to make small tweaks to your home to avoid falls. This can include cleaning rooms to avoid tripping hazards, using sticky shower mats, and holding rails when you walk.
Nutrition: A balanced diet can accelerate recovery in various ways following a concussion. Prioritize foods that are high in healthy, unsaturated fat and rich in antioxidants. Consider supplementing fish oil, turmeric, and electrolytes to accelerate the natural healing process that occurs within the first few months of recovery.
Sprint Mentality vs. Marathon Mentality: Many find adopting more of a sprint mentality throughout the day helpful. This means dedicating small chunks of time to focus exclusively on getting things done and then allowing the system to recover. Not only will this help you stay on task and improve productivity, but it will also give your brain the rest it needs to recover and avoid a crash.
Avoid Excessive Caffeine, Nicotine, and Alcohol: During concussion recovery, avoid these 3 things until your symptoms have stabilized. Caffeine and alcohol naturally cause the body to shed water, leading to dehydration and electrolyte imbalances. Nicotine tends to ramp up anxiety, which is usually present in post-concussion dizziness.
Conclusion
Post-concussion dizziness is a common complaint with a variety of options for treatment. Be sure to do your homework and find a provider to carefully evaluate your situation before recommending treatment. Be patient and realize that recovery from concussions is rarely a straight line.
If you have questions about concussion recovery, click here to schedule a complimentary consultation with one of our doctors. We’ve treated hundreds of complex neurologic cases and can help piece together the missing pieces in your recovery.
*Note: The information provided in this article is for educational purposes only and does not constitute a doctor-patient relationship. Patients should consult their medical provider or primary care physician before trying any remedies or therapies at home.

